








































Preview text:
CÁ C C Á C MẶ M T Ặ T CẮ C T C Ắ Ơ B T C Ả Ơ B N S N IÊU ÂM TIM QU M A TIM QU THÀNH THÀN NGỰ N C GỰ BS. P h P ạ h m m Q uang Hu g y Hu
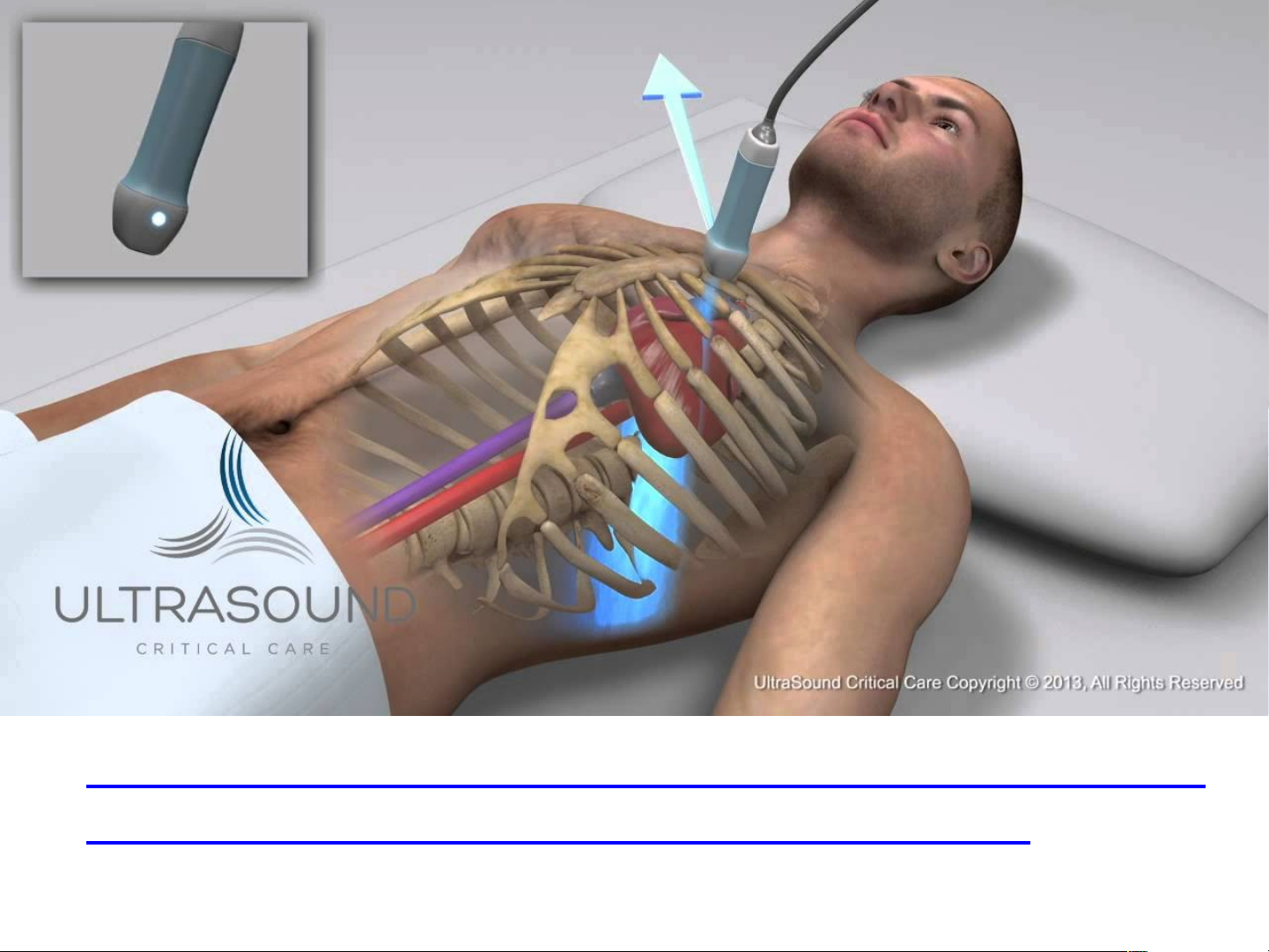
Caùc vò trí cuûa ñaàu doø ôû caùc ñöôøng caét: ñöôøng caét
caïnh öùc beân traùi (A); ñöôøng caét töø moûm tim (B);
ñöôøng caét döôùi söôøn (C); ñöôøng caét treân hoõm öùc (D) A B D C 1.Pa P r a a r st s e t r e nal Long-Ax A i x s View ie (PLAX V LA ie X V w) ie
• Transducer position: left sternal edge; 2nd–4th space
• Marker dot direction: points towards right shoulder.
How to obtain- Parasternal Long Axis Ultrasound
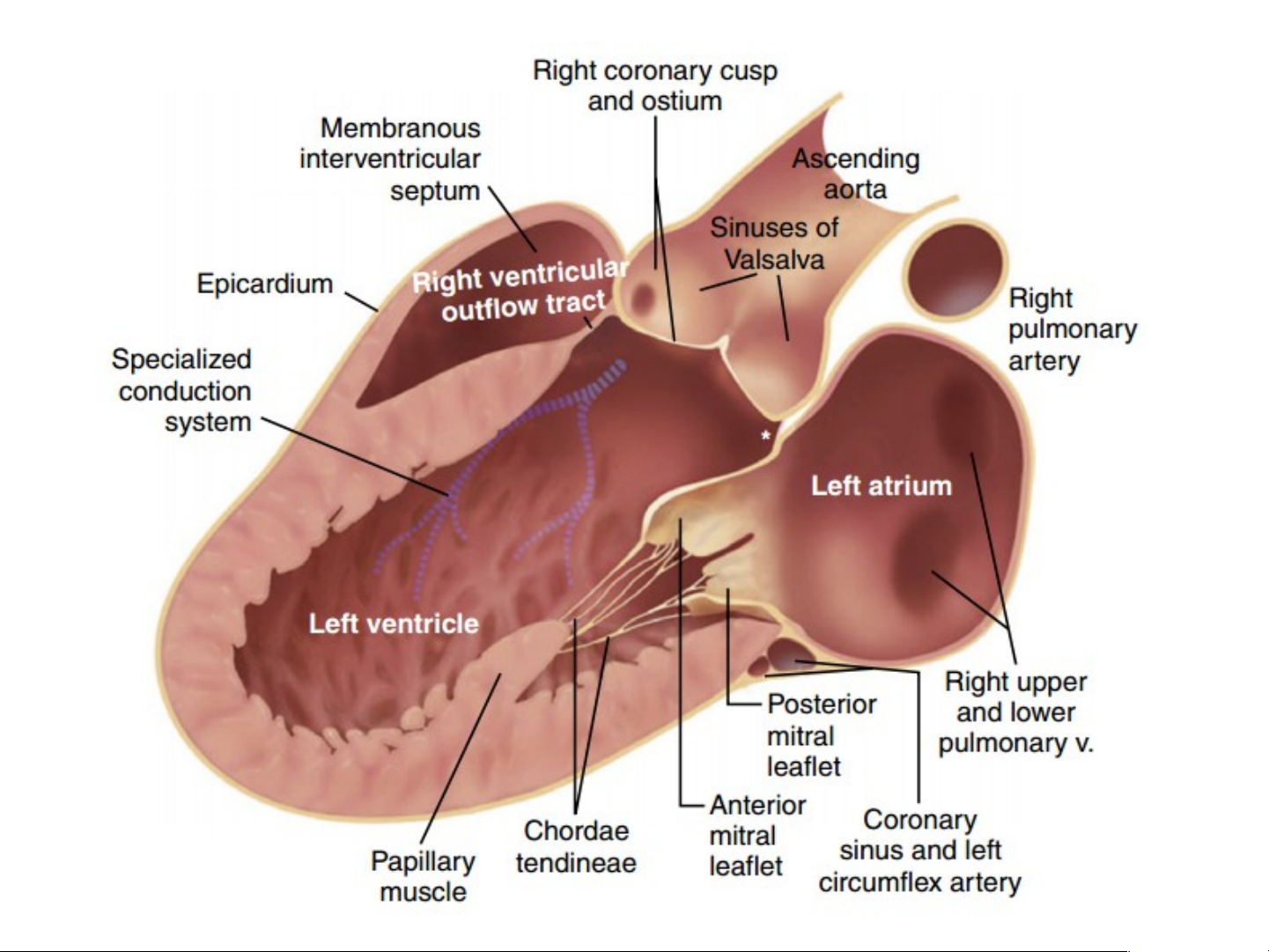
View - Training and Techniques - ICU.mp4 • Structures seen: – proximal aorta – aortic valve – left atrium – mitral valve – left ventricle – IV septum – posterior wall – right ventricle – pericardium.
@Most echo studies begin with this view. It sets
the stage for subsequent echo views
Normal parasternal longaxis 2D echo images. End-diastolic (left) and end-systolic
(right) images show the anatomic features seen in previous Figure . In
addition, the descending thoracic aorta (DA) is seen posterior to the left atrium. Aorta M-Mode Mitral M-Mode M mode LV measurements
• Open the QR code reader application on your mobile device.
• Point the device’s camera at the code and scan.
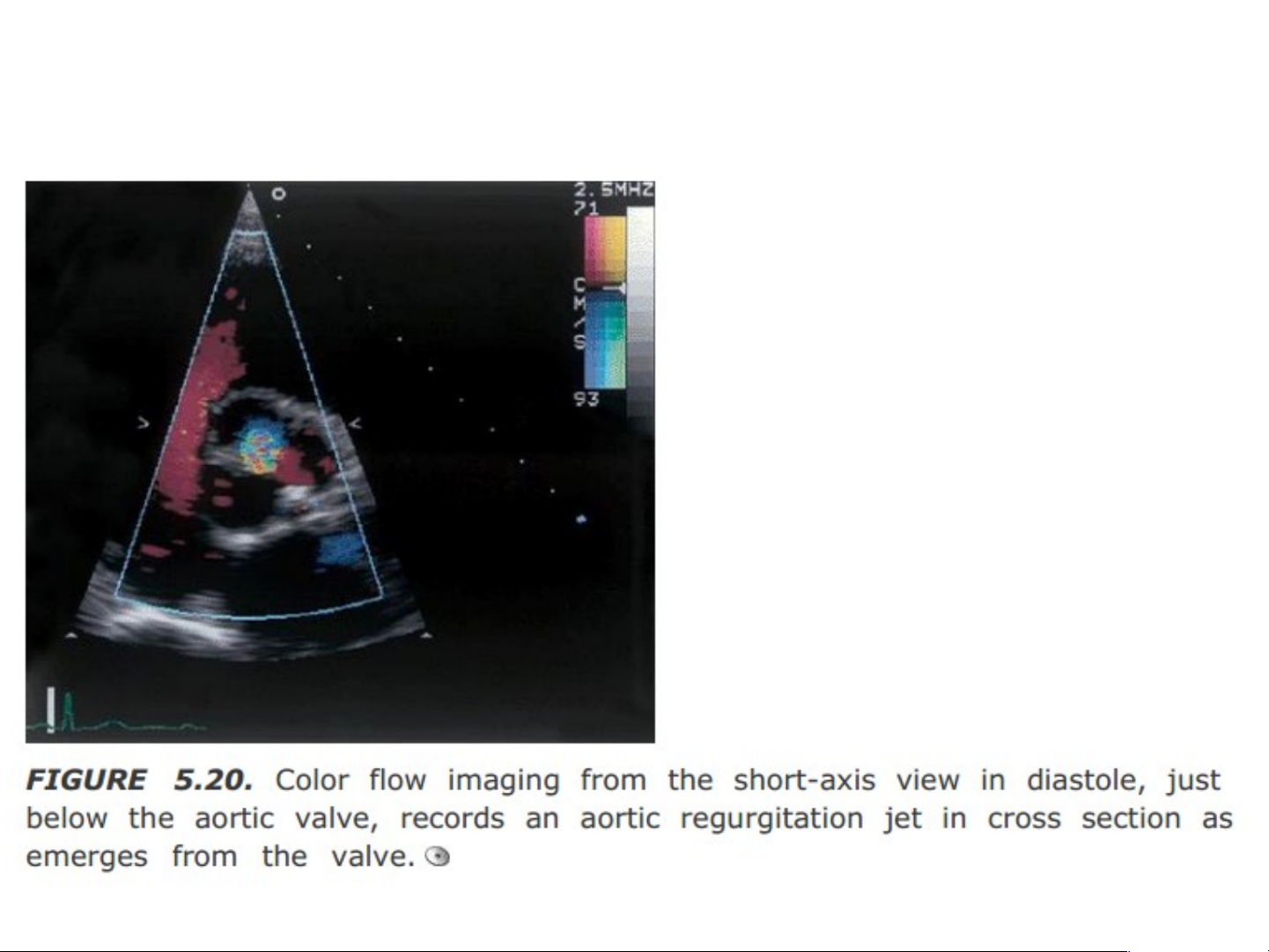
• Each code opens an individual video player for instant viewing—no log-on required 2. P . a P ra r s a t s e t rnal S na hort- t Ax A i x s View ie s w (PSA S X V A i X V ew e s w )
• Transducer position: left sternal edge; 2nd–4th space
• Marker dot direction: points towards left shoulder (90° clockwise from PLAX).
• By tilting the transducer on an axis between the left
hip and right shoulder, short-axis cuts are obtained at
different levels, from the aorta to the LV apex.
• This angulation of the transducer from the base to
apex of the heart for short-axis views is known as “bread-loafing”.
How to obtain- Parasternal Short Axis Ultrasound View - Traini ng and Techniques - ICU.mp4
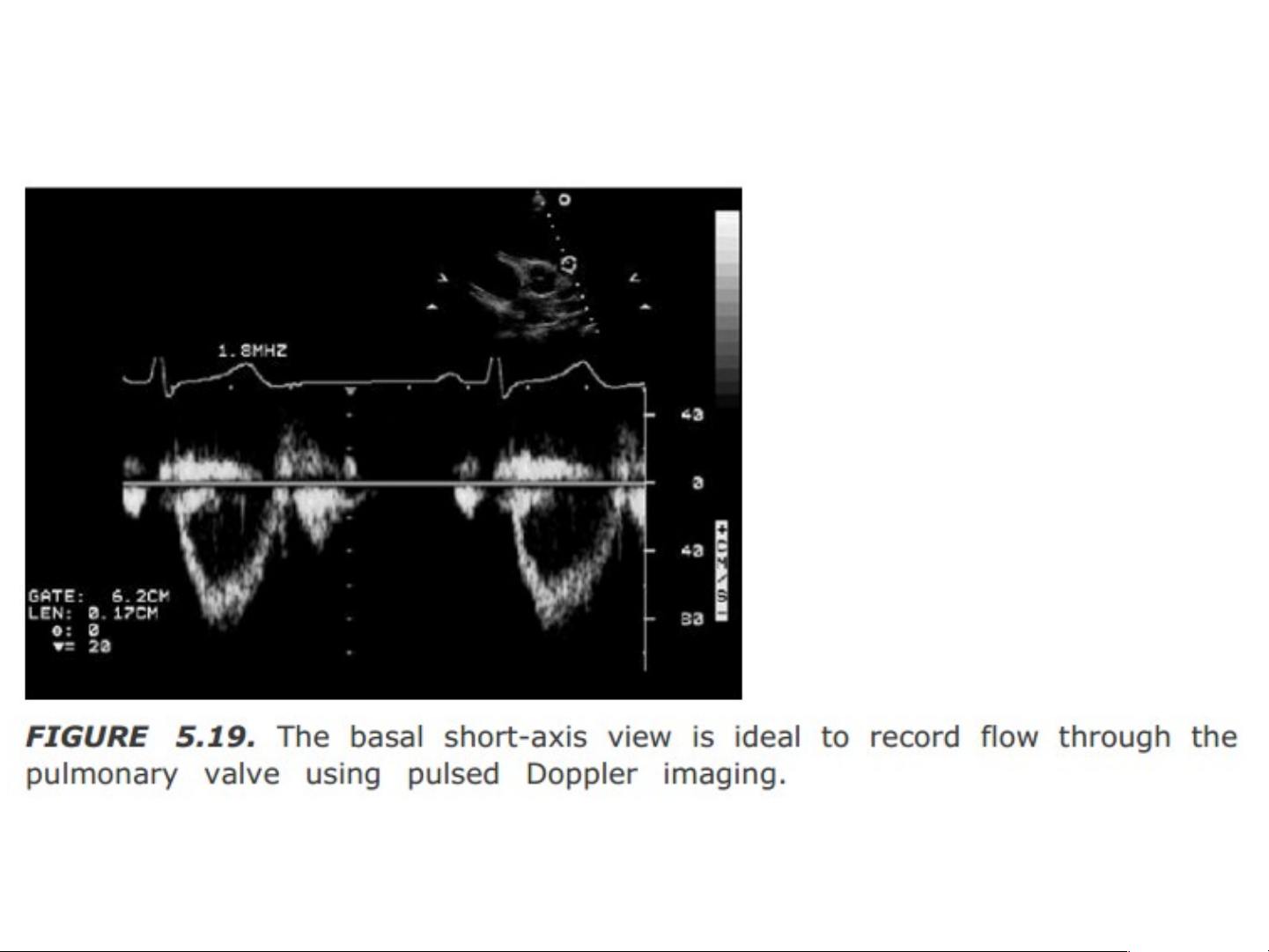
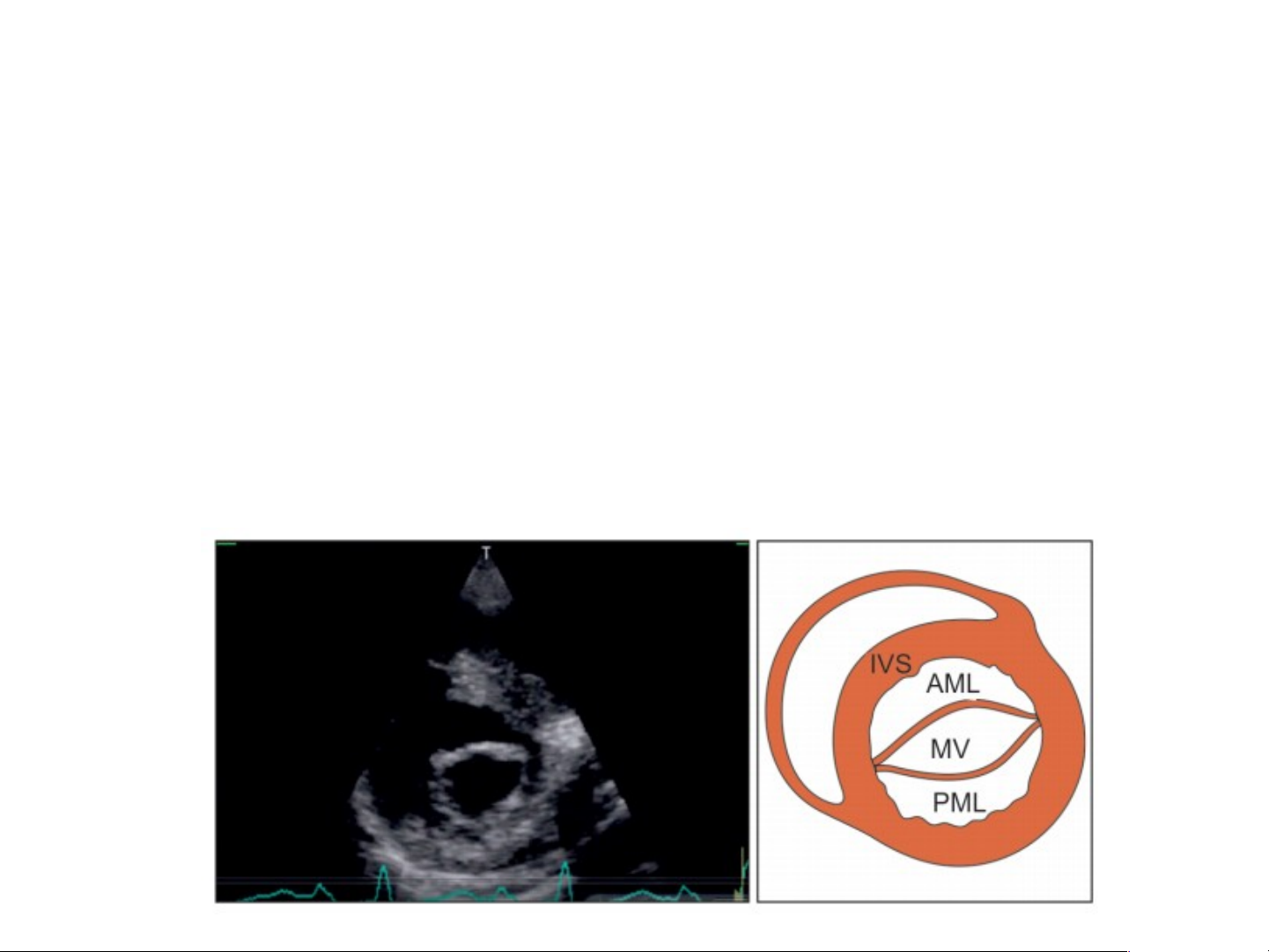
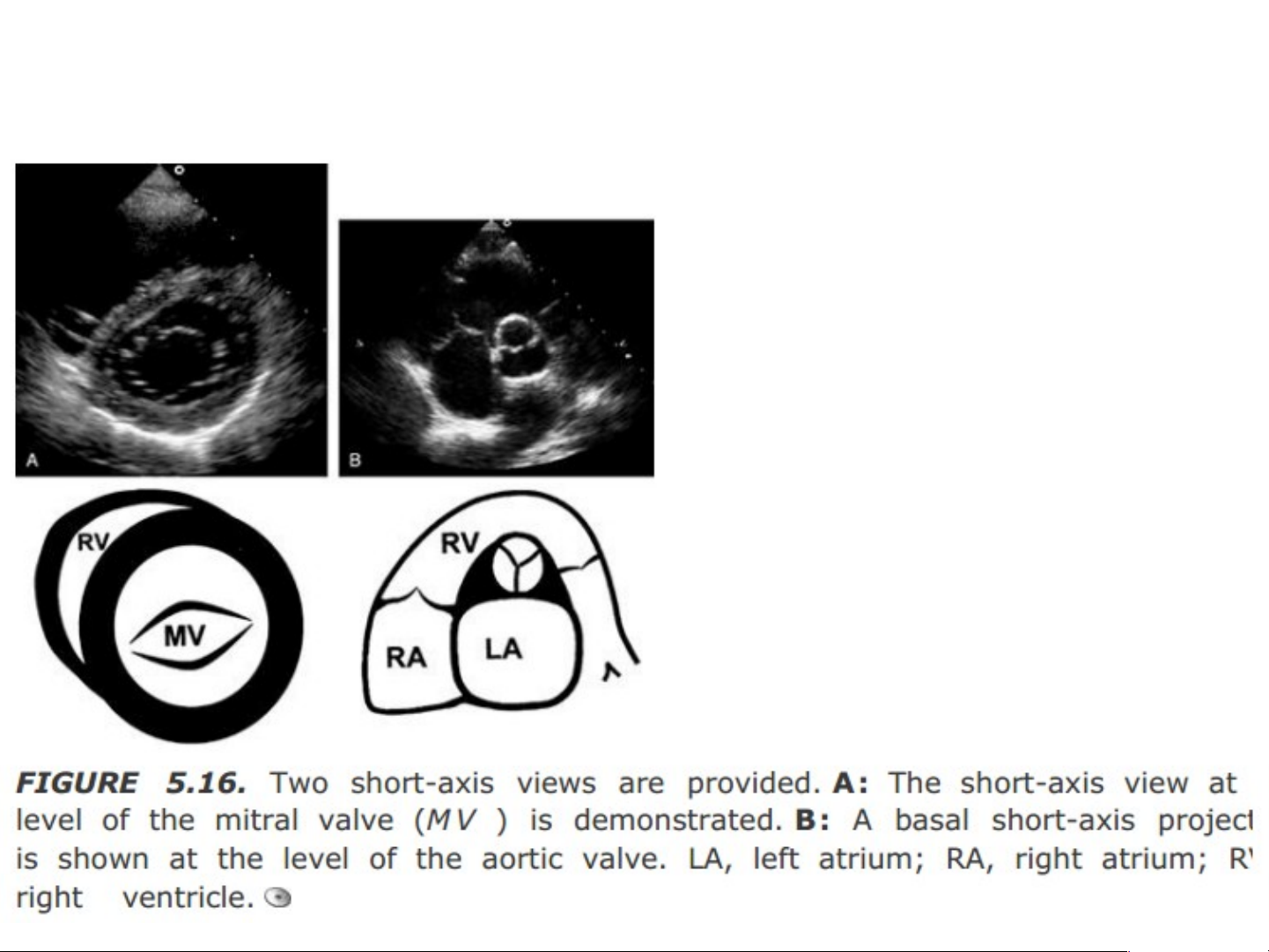
The parasternal short-axis (PSAX) views Pulmonary Artery (PA) Level • Structures seen: – pulmonary artery – pulmonary valve – RV outflow tract. Aortic Valve (AV) Level • Structures seen: – aortic valve cusps – left atrium – interatrial septum – tricuspid valve – RV outflow tract. Mitral Valve (MV) Level • Structures seen: – mitral valve orifice – mitral valve leaflets – ventricular septum Papillary Muscle (PM) Level • Structures seen: - anterolateral PM (3o) - posteromedial PM (7o) - anterior wall (12o to 3o) - lateral wall (3o to 6o) - inferior wall (6o to 9o) - IV septum (9o to 12o) 3. A 3. pi A ca c l 4-Chambe l 4-Cha r mbe View ie (A4C (A H V 4C iew) ie
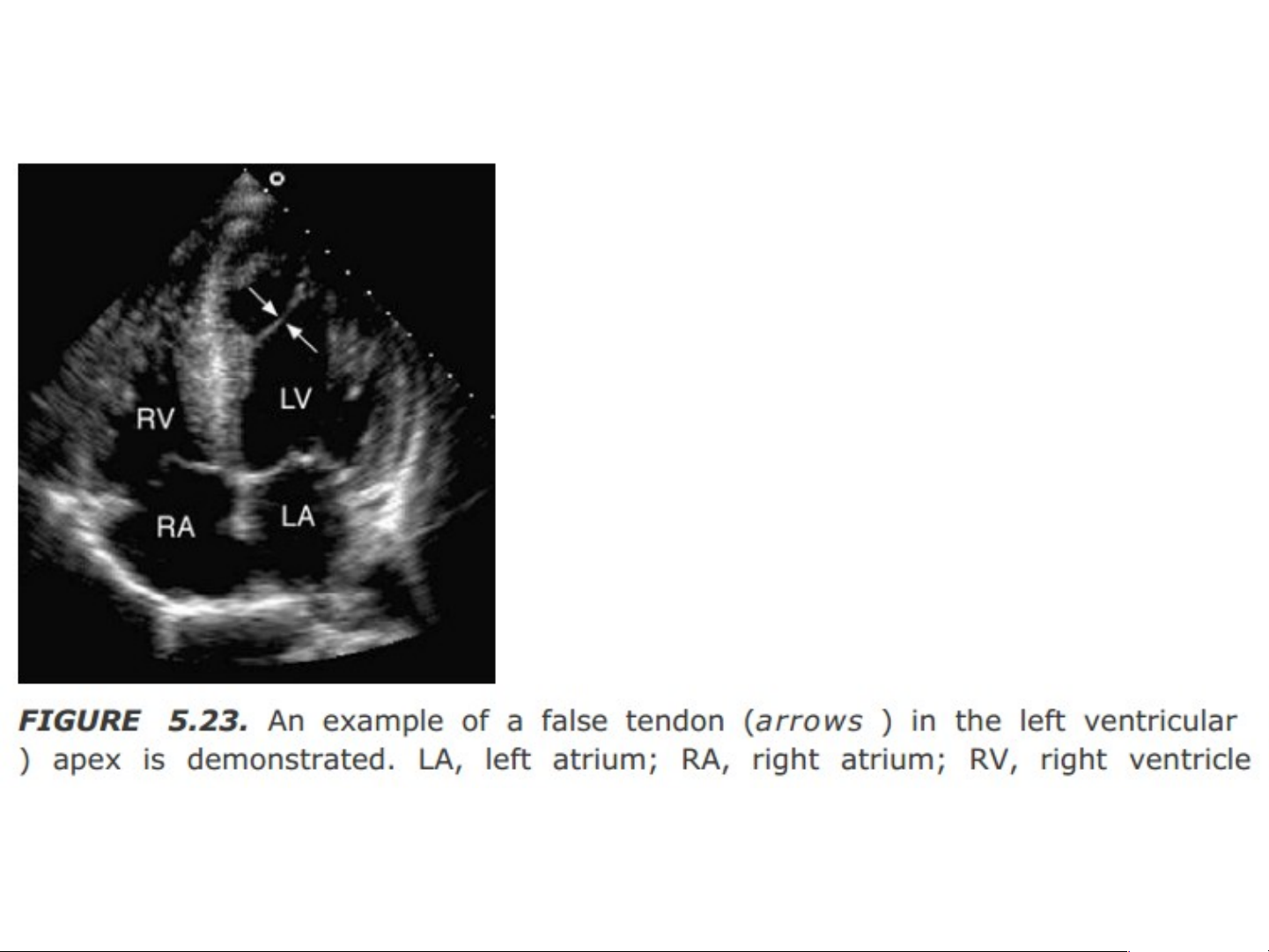
• Transducer position: apex of the heart
• Marker dot direction: points towards left shoulder. • Structures seen: – right and left ventricle – right and left atrium – mitral, tricuspid valves – IA and IV septum – left ventricular apex
– lateral wall left ventricle – free wall right ventricle
How to obtain- Apical 4 (Four) Chamber Ultrasou
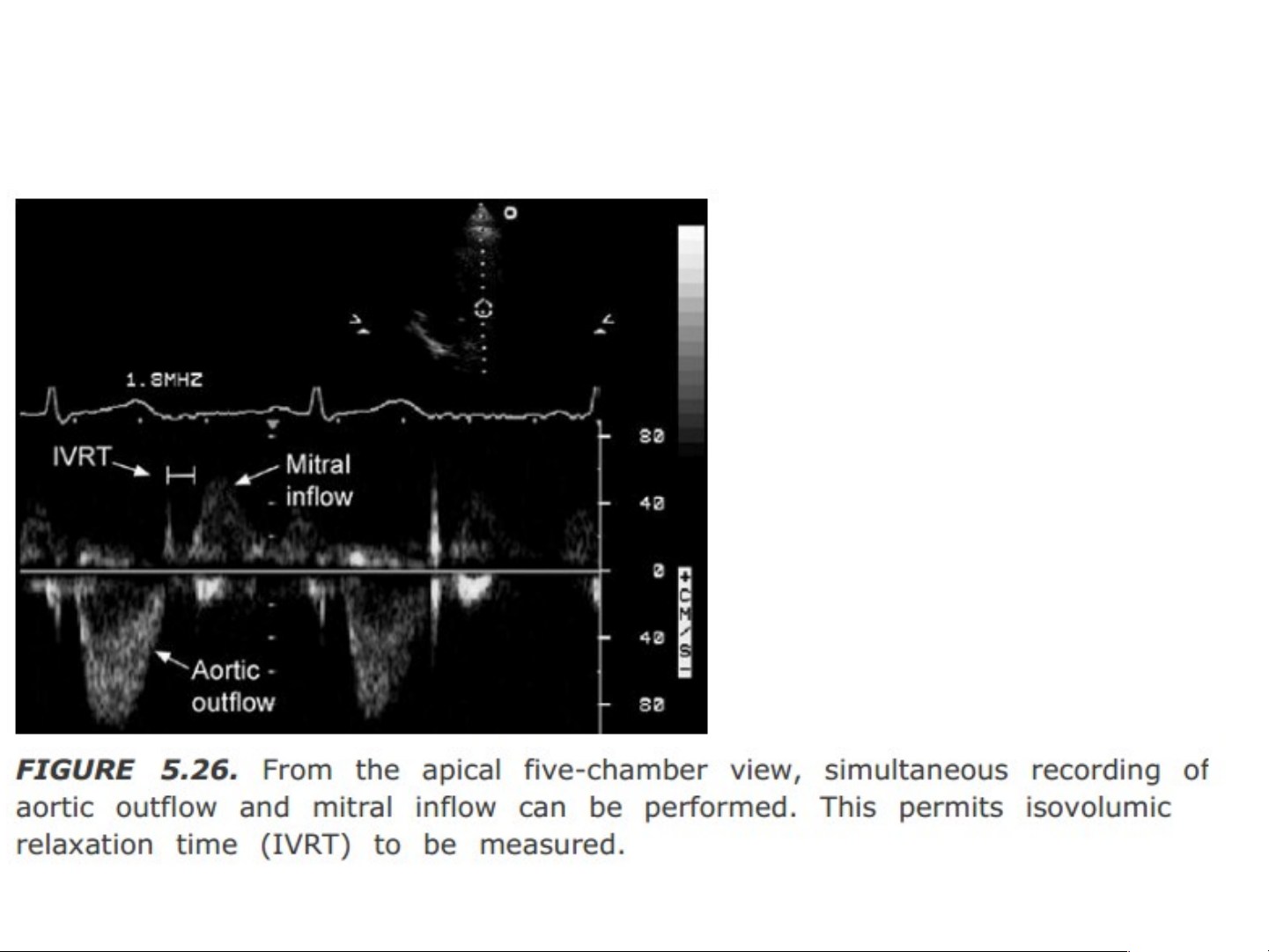
nd View- Training and Techniques - ICU.mp4 4. A 4. pi A ca c l 5-Chambe l 5-Cha r mbe View ie (A5C A H vie 5C w) H vie
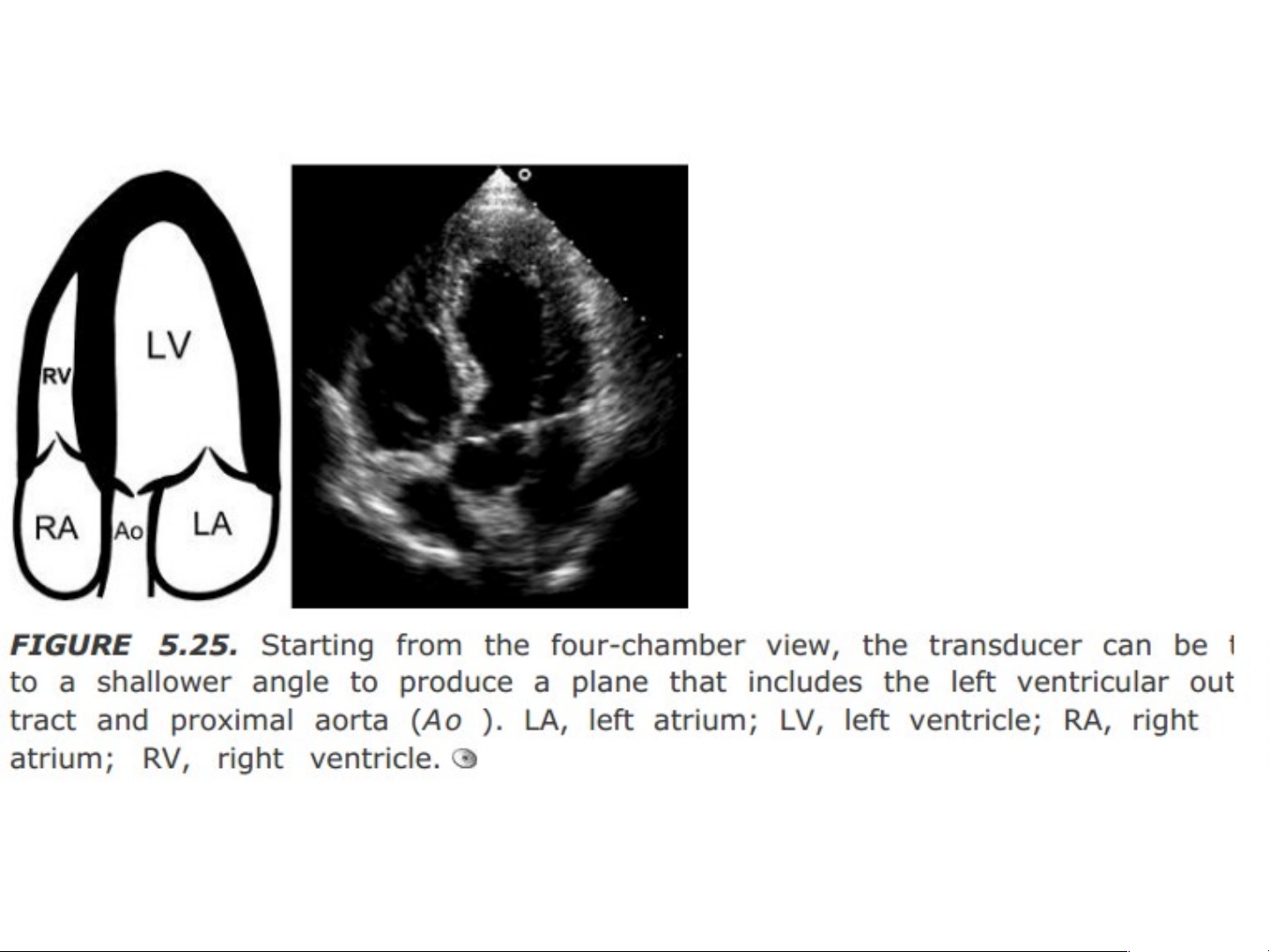
• The A5CH view is obtained after the A4CH
view by slight downward tilting of the
transducer. The 5th chamber added is the left
ventricular outflow tract (LVOT).
• Transducer position: as in A4CH view.
• Marker dot direction: as in A4CH view. • Structures seen:
As in A4CH view. Additionally: — LV outflow tract — aortic valve — proximal aorta. 5. T w T o w & T & hree hr Chamber Vie V w ie 6. S ubco c st s a t l V l ie V w ie
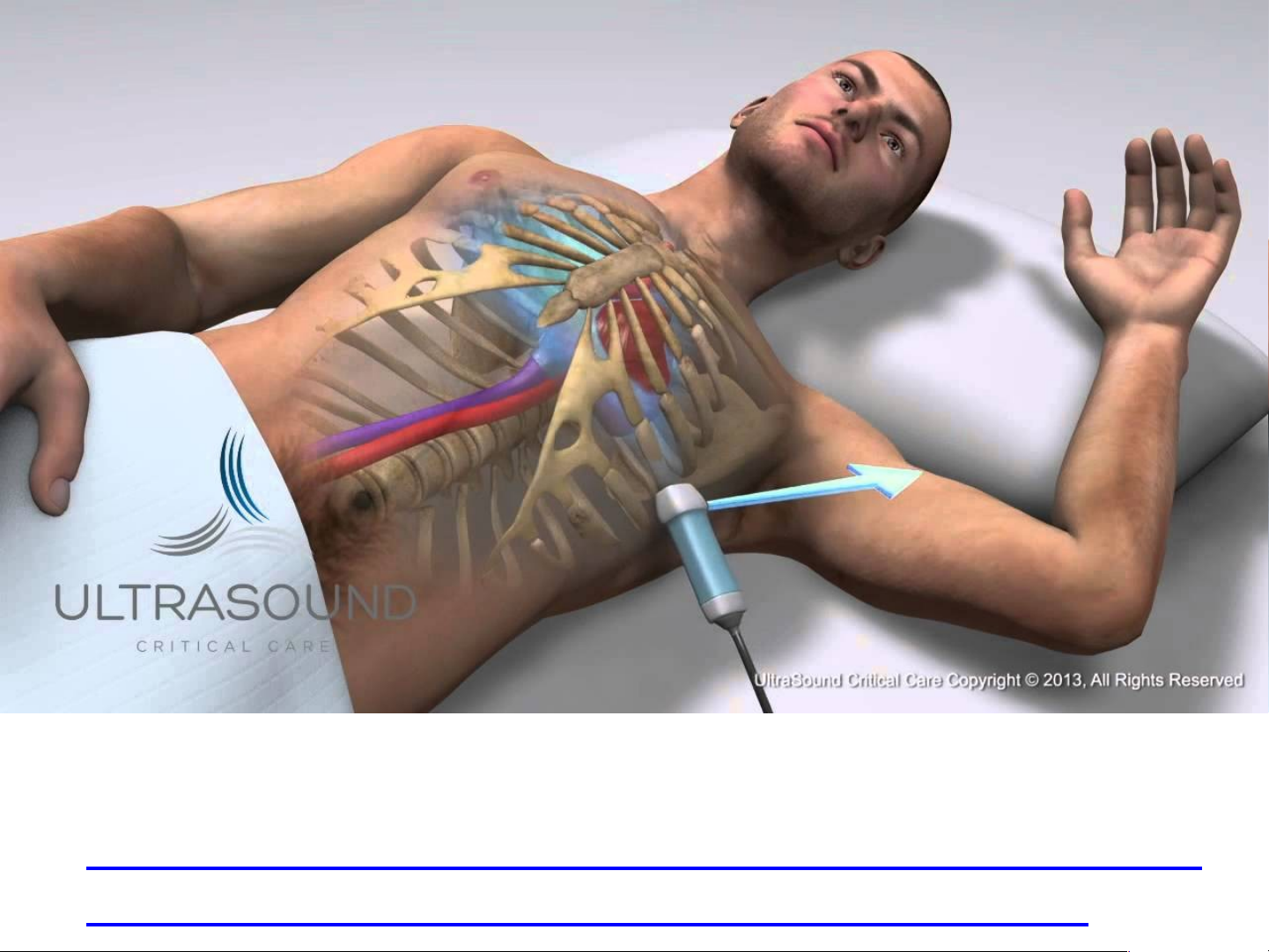
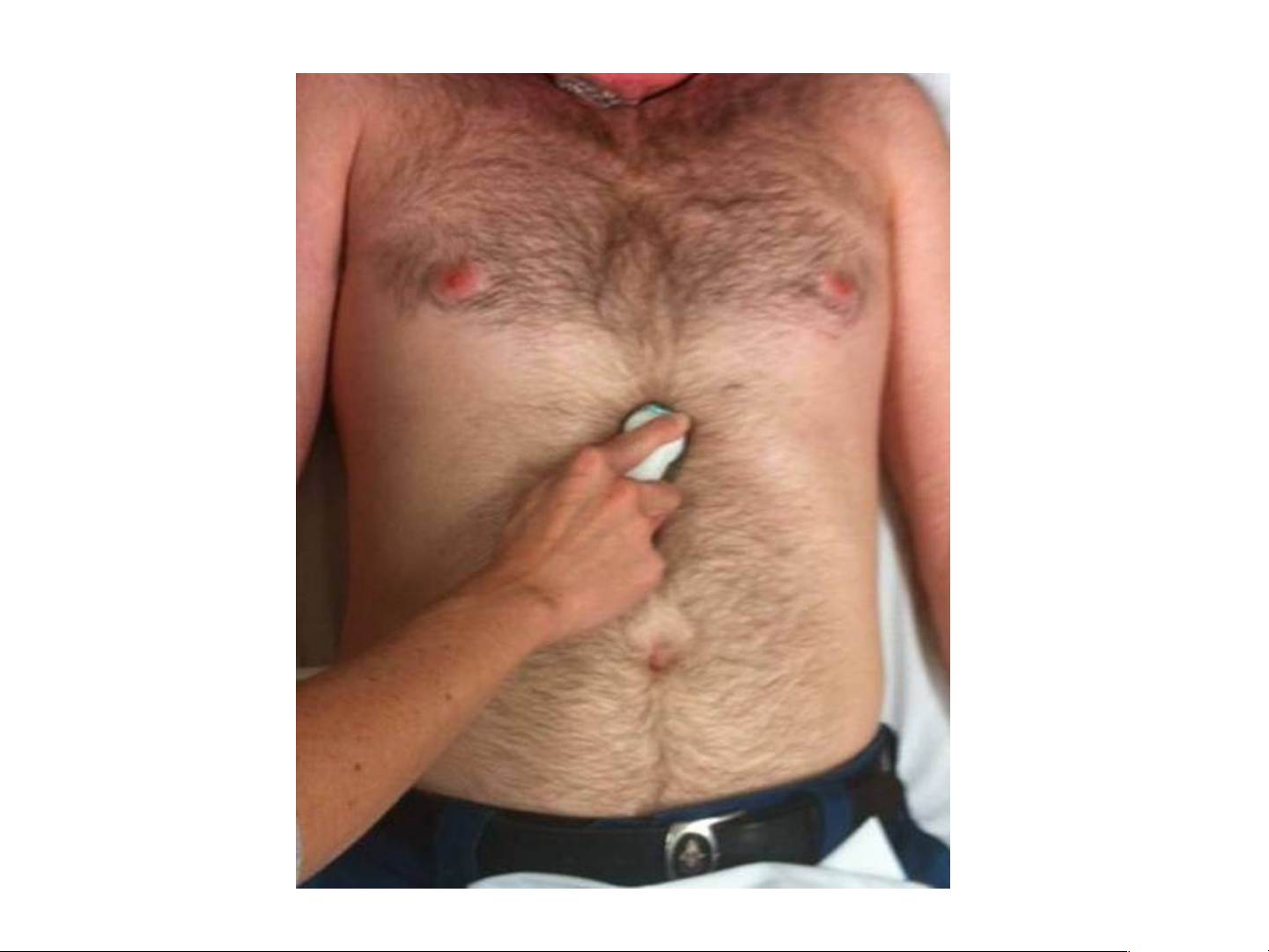
• For subcostal view, the position of the subject is
different from that used to obtain parasternal and apical views.
• The subject lies supine with the head held slightly low,
feet planted on the couch and the knees slightly flexed.
• Better images are obtained with the abdomen relaxed
and during the phase of inspiration.
• Transducer position: under the xiphisternum
• Marker dot position: points towards left shoulder. • Structures seen: As in A4CH view.
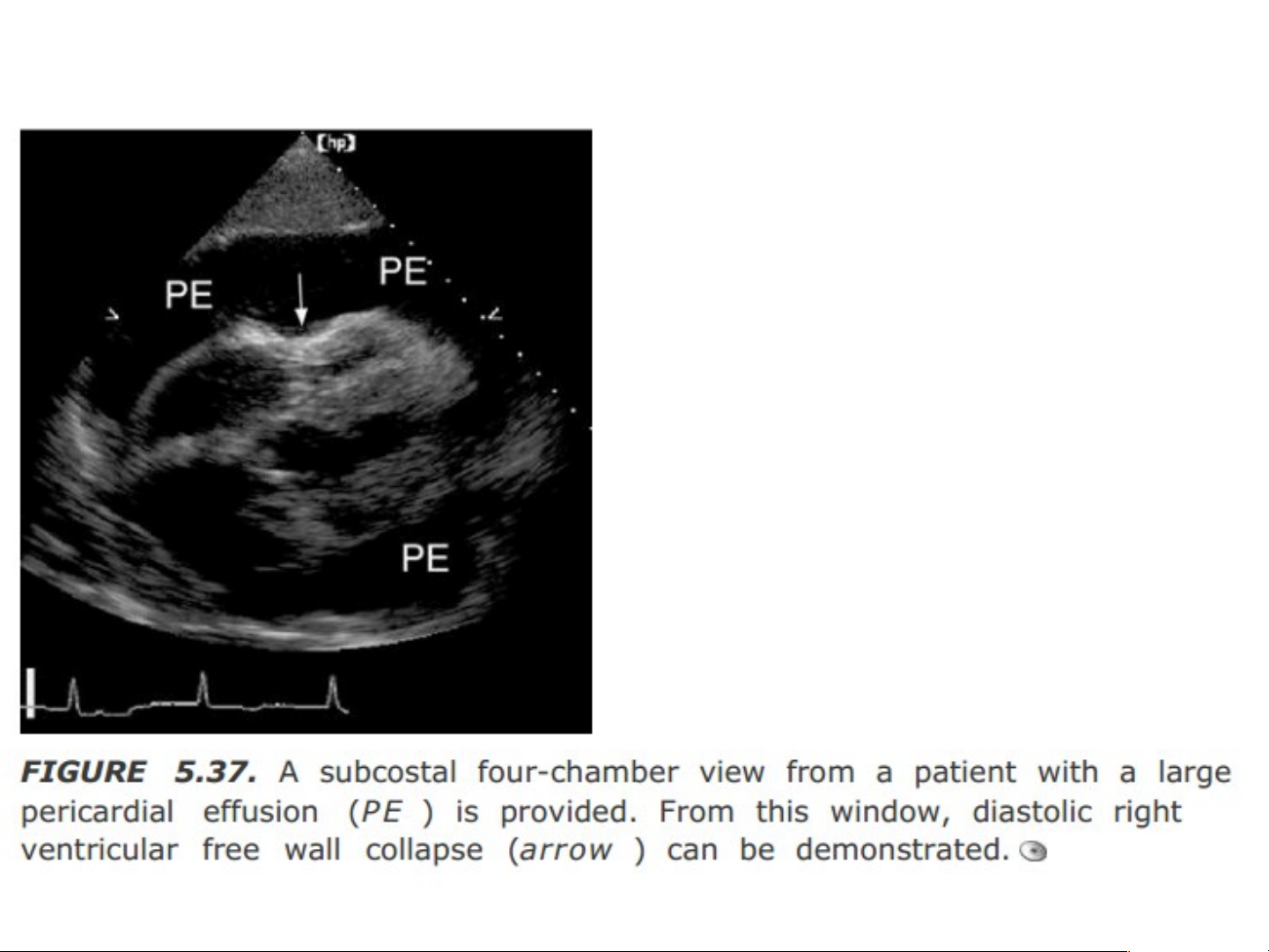
• The subcostal view is particularly useful when
transthoracic echo is technically difficult because of the following reasons: – severe morbid obesity – chest wall deformity – pulmonary emphysema.
• The following structures are better seen from the
subcostal view than from the apical 4-chamber view: – inferior vena cava – descending aorta – interatrial septum – pericardial effusion.
Maët caét 5 buoàng döôùi söôøn A B C
Maët caét döôùi söôøn truïc ngang cho
thaáy ÑMP baét nguoàn töø thaát phaûi C
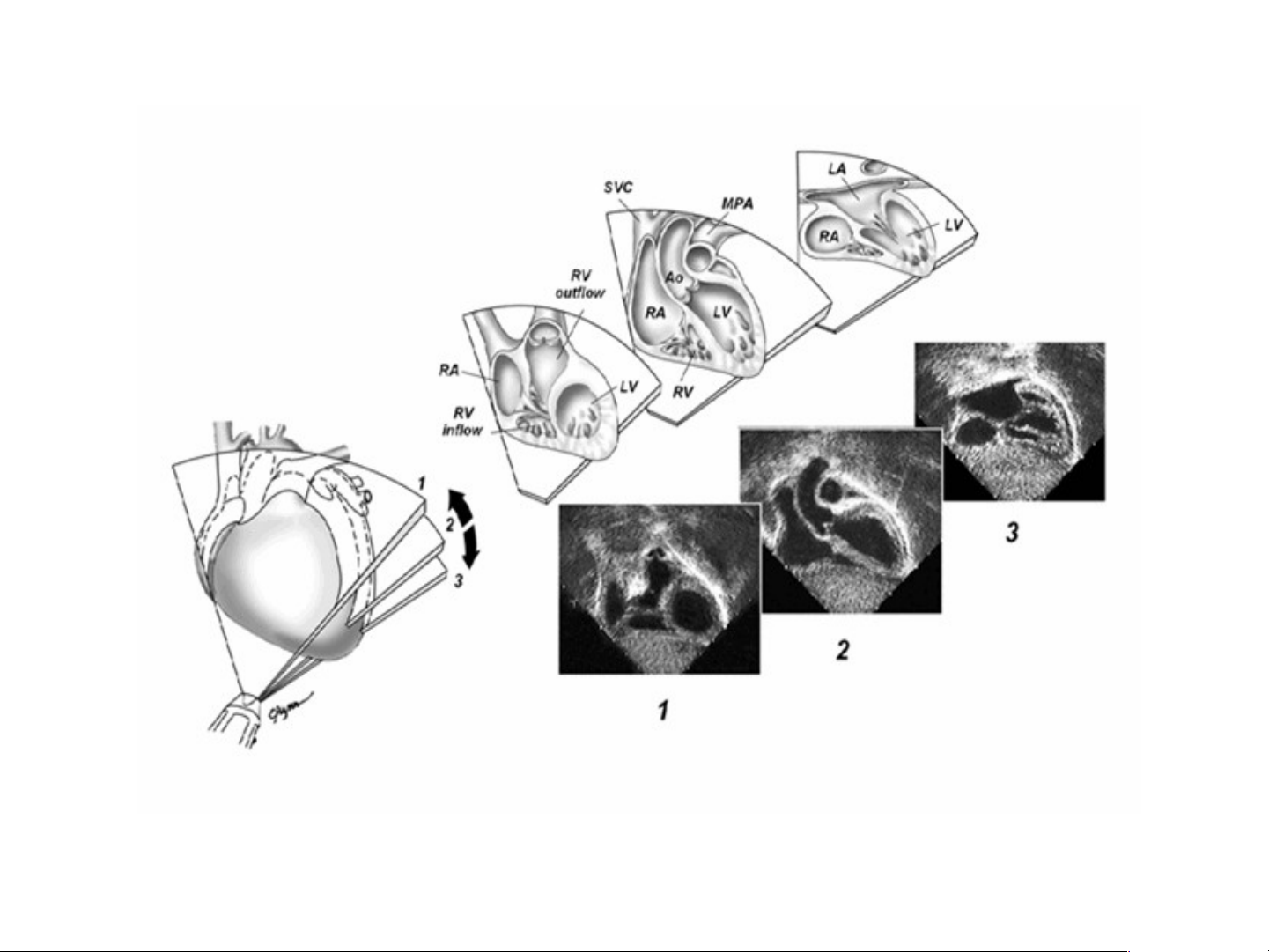
Mặt cắt quét dưới mũi ức trục dài •
1, Tâm thất phải (RV), buồng chứa và đường thoát ra được nhìn thấy với van động mạch phổi. •
2, Với gập góc đầu dò, trục dài của tâm thất trái (LV), van động mạch chủ (Ao), và phần Ao lên được nhìn
thấy. Tĩnh mạch chủ trên (SVC) được nhìn thấy bên phải của Ao lên, động mạch phổi chính (MPA) được
nhìn thấy. Kết nối của SVC tới tâm nhĩ phải (RA) được thể hiện. •
3, Khi đầu dò gắp góc tiếp với bụng, vách liên nhĩ và hai tĩnh mạch phổi đổ vào tâm nhĩ trái (LA) được nhìn thấy.
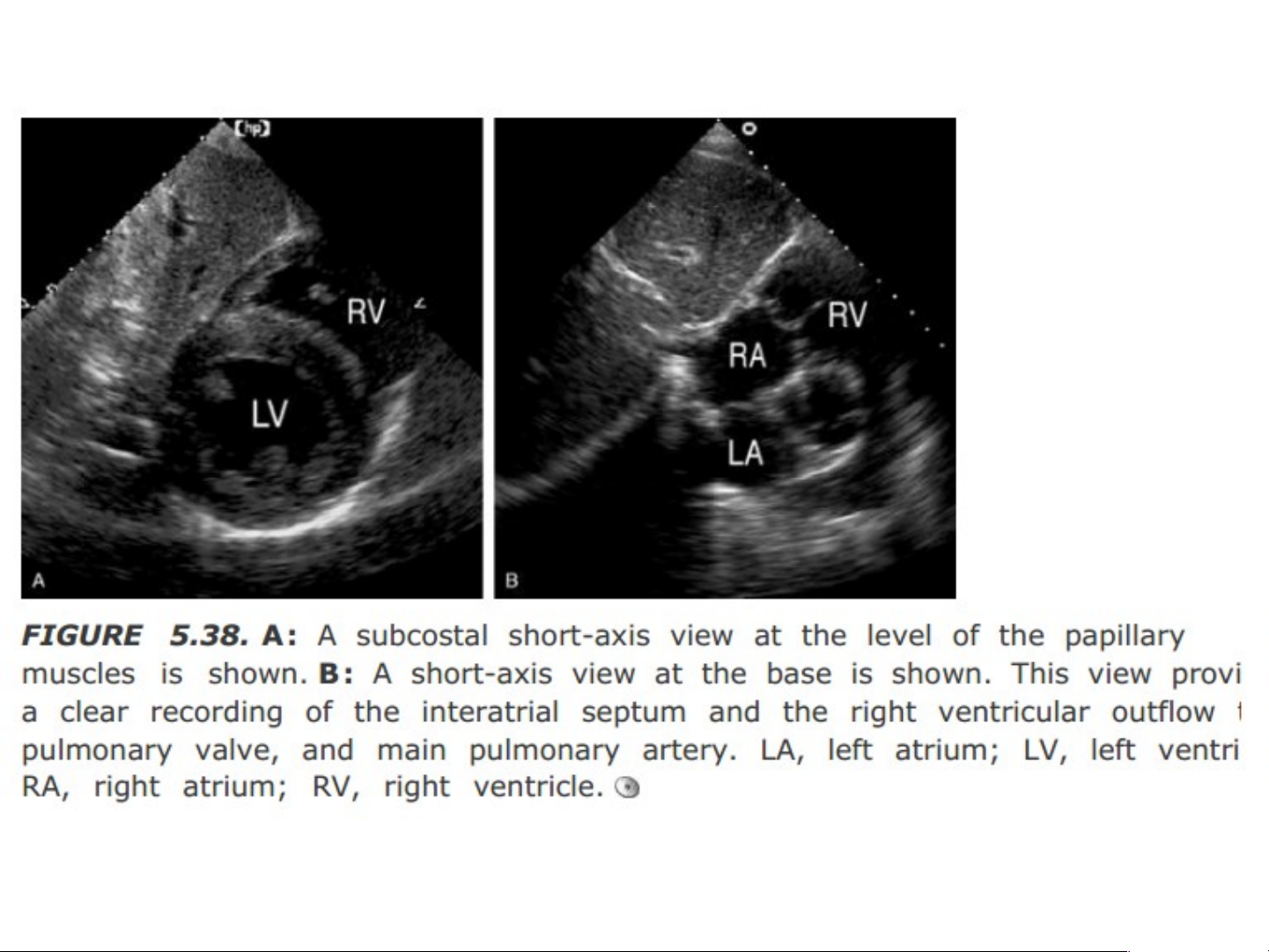
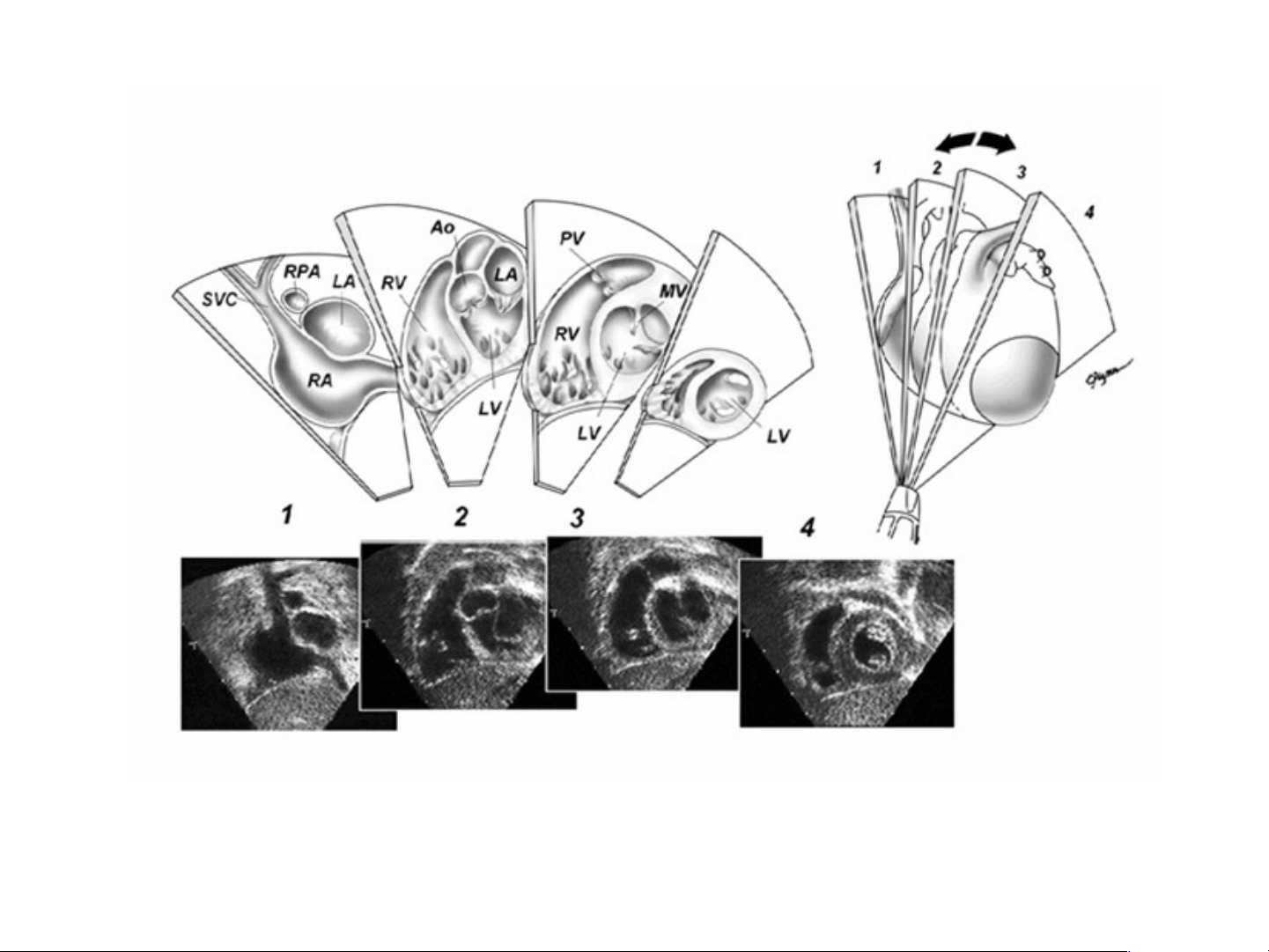
Mặt cắt quét dưới mũi ức trục ngắn
1, Tại mặt cắt hướng cạnh phải của tim, tĩnh mạch chủ trên (SVC) và tĩnh mạch chủ dưới đi vào tâm nhĩ phải
(RA). Động mạch phổi phải (RPA) được nhìn thấy trong mặt cắt ngang phía sau SVC và ở trên tâm nhĩ trái (LA).
2, Với góc gập ở về bên trái, tâm thất trái (LV) tâm thất phải (RV) và các van nhĩ thất được nhìn thấy. Van động
mạch chủ (Ao) được nhìn thấy trong mặt cắt ngang ở cấp độ này.
3, thêm gập góc về bên trái cho thấy mặt cắt ngang điểm của LV và van hai lá (MV), đường ra RV van động mạch phổi (PV).
4, Quét đầu dò tiếp giữa hai thất, quan sát vách ngăn và cột cơ LV, với phần đỉnh của cả hai tâm thất. 7. Supras r t as e t rnal Vie nal V w ie
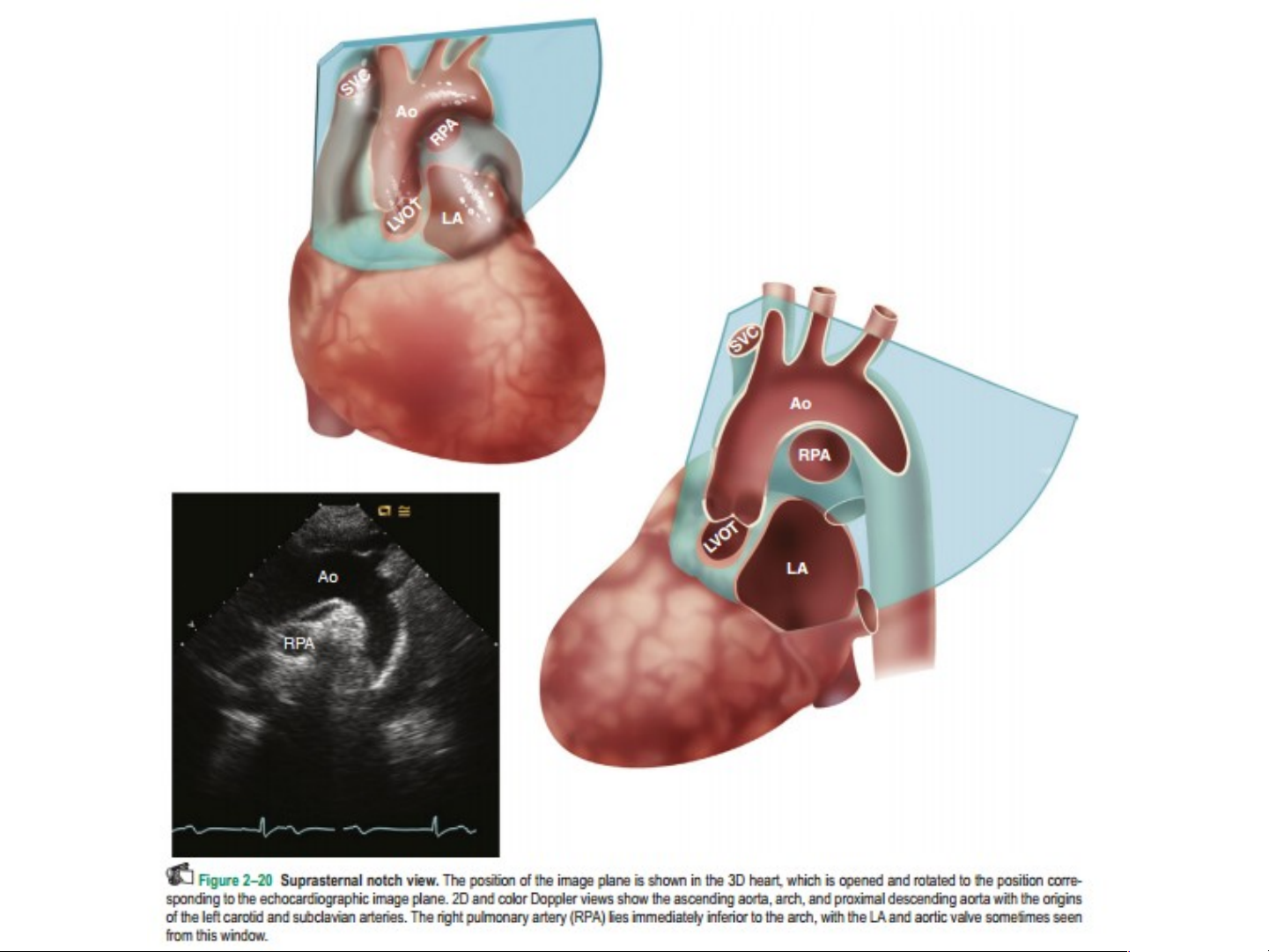
• For suprasternal view, the subject lies supine with the neck
hyperextended by placing a pillow under the shoulders. The
head is rotated slightly towards the left.
• The position of arms or legs and the phase of respiration have
no bearing on this echo window.
• Transducer position: suprasternal notch.
• Marker dot direction: points towards left jaw. • Structures seen: – ascending aorta – pulmonary artery.
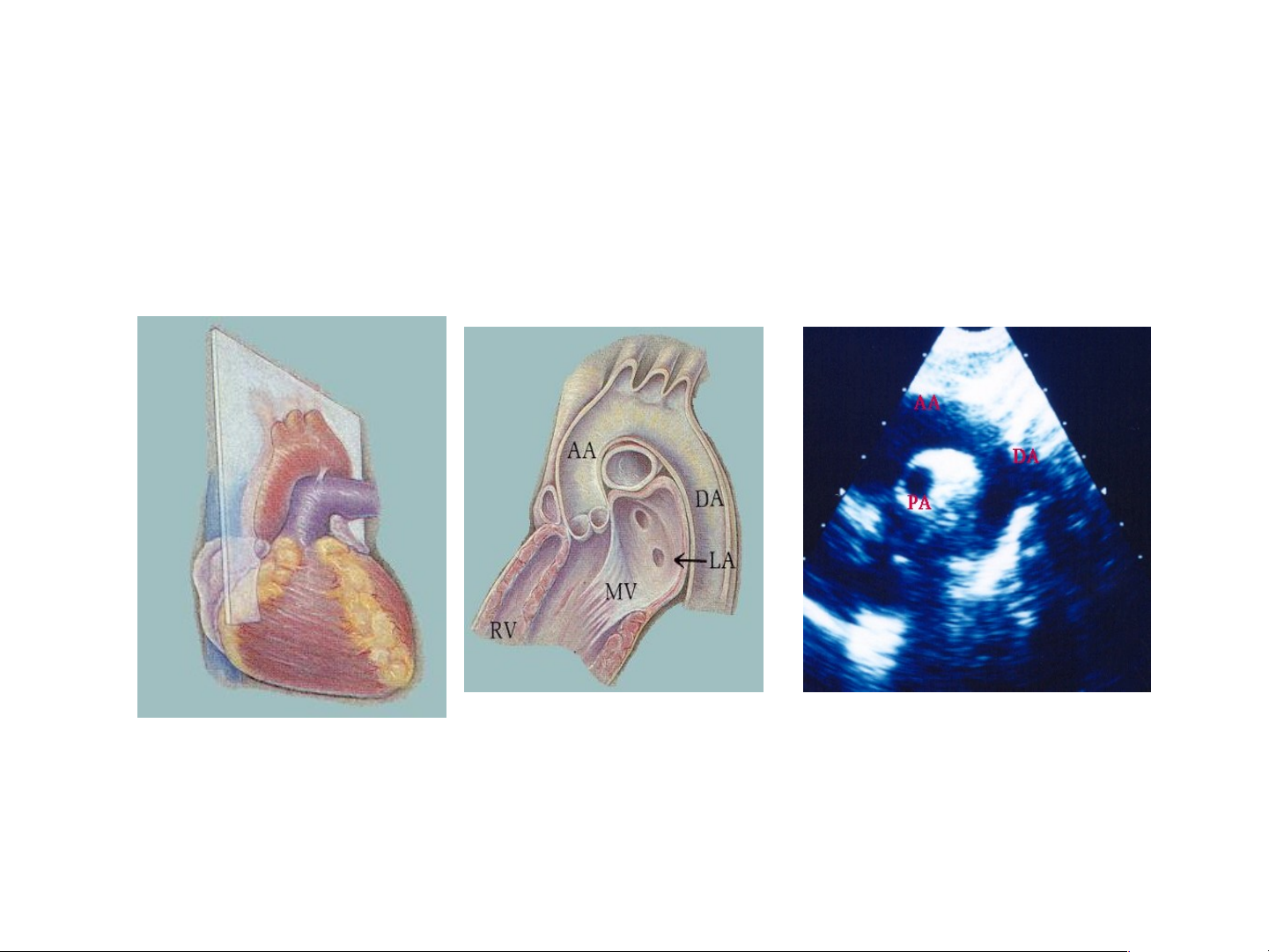
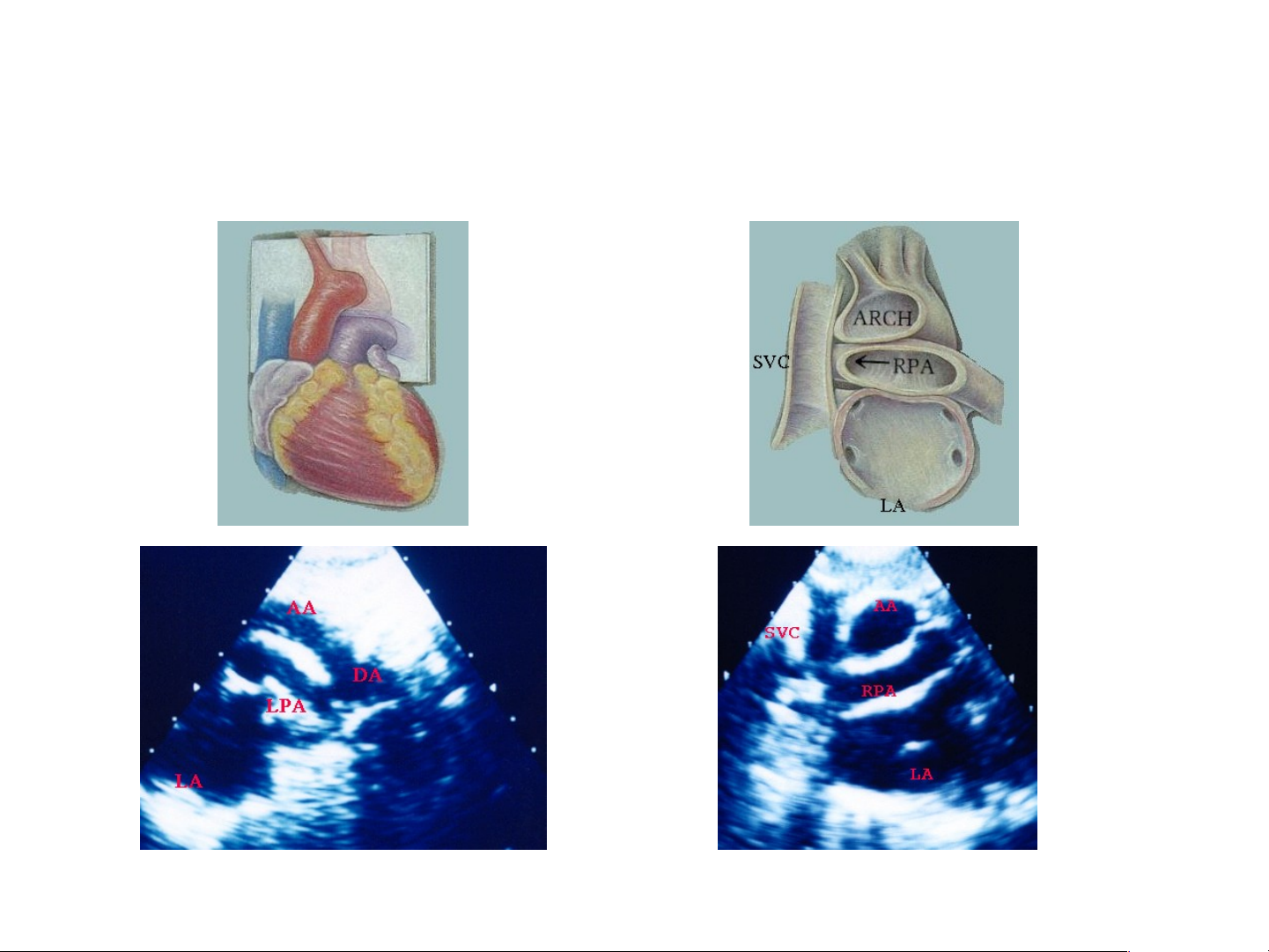
Maët caét treân hoõm öùc cô baûn theo truïc doïc
giuùp thaáy ÑMC leân, cung ÑMC, ÑMC xuoáng vaø ÑMP (B,C) A B C
Maët caét treân hoõm öùc hôi nghieâng ñaàu doø giuùp thaáy cung
ÑMC (AA), ÑMC xuoáng (DA), ÑMP traùi (LPA) (C). Xoay ñaàu doø 900
giuùp thaáy: ÑMC caét ngang (AA), ÑMP caét doïc (RPA),tónh maïch chuû treân (SVC) (D) A B C D 8. R . i R ght h P a P r a as r t as er t na n l a Vi ew e
• For right parasternal view, the subject lies in the semirecumbent
position on the right side. The right arm is tucked under the
head and the left arm lies along the left side of the body.
• In other words, this position is the mirror-image of that used for the left parasternal view.
• Transducer position: right sternal edge; 2nd–4th space
• Marker dot direction: points towards left shoulder. • Structures seen: – aortic valve – aortic root. Tài liệu tham khảo
• Phaïm Nguyeãn Vinh vaø c/s. Atlas sieâu
aâm tim 2D vaø Doppler maøu. NXB Y hoïc 2000
• Atul Luthra - Echo made easy, 3rd editon.
• Harvey Feigenbaum et al - Feigenbaum’s Echocardiography, 7th edition.
• Catherine M.Otto – Textbook of clinical echocardiography, 5th edition.
• Guidelines for pediatric echocardiography-
American Society of Echocardiography. Thank Tha you for y o our our at a tention
Document Outline
- Slide 1
- Slide 2
- Slide 3
- Slide 4
- 1.Parasternal Long-Axis View (PLAX View)
- Slide 6
- Slide 7
- Slide 8
- Slide 9
- Slide 10
- Aorta M-Mode
- Mitral M-Mode
- M mode LV measurements
- Slide 14
- Slide 15
- Slide 16
- Slide 17
- 2. Parasternal Short-Axis Views (PSAX Views)
- Slide 19
- Slide 20
- Pulmonary Artery (PA) Level
- Aortic Valve (AV) Level
- Slide 23
- Slide 24
- Slide 25
- Slide 26
- Slide 27
- Mitral Valve (MV) Level
- Slide 29
- Slide 30
- Papillary Muscle (PM) Level
- Slide 32
- Slide 33
- Slide 34
- Slide 35
- 3. Apical 4-Chamber View (A4CH View)
- Slide 37
- Slide 38
- Slide 39
- Slide 40
- Slide 41
- Slide 42
- Slide 43
- Slide 44
- Slide 45
- Slide 46
- 4. Apical 5-Chamber View (A5CH view)
- Slide 48
- Slide 49
- Slide 50
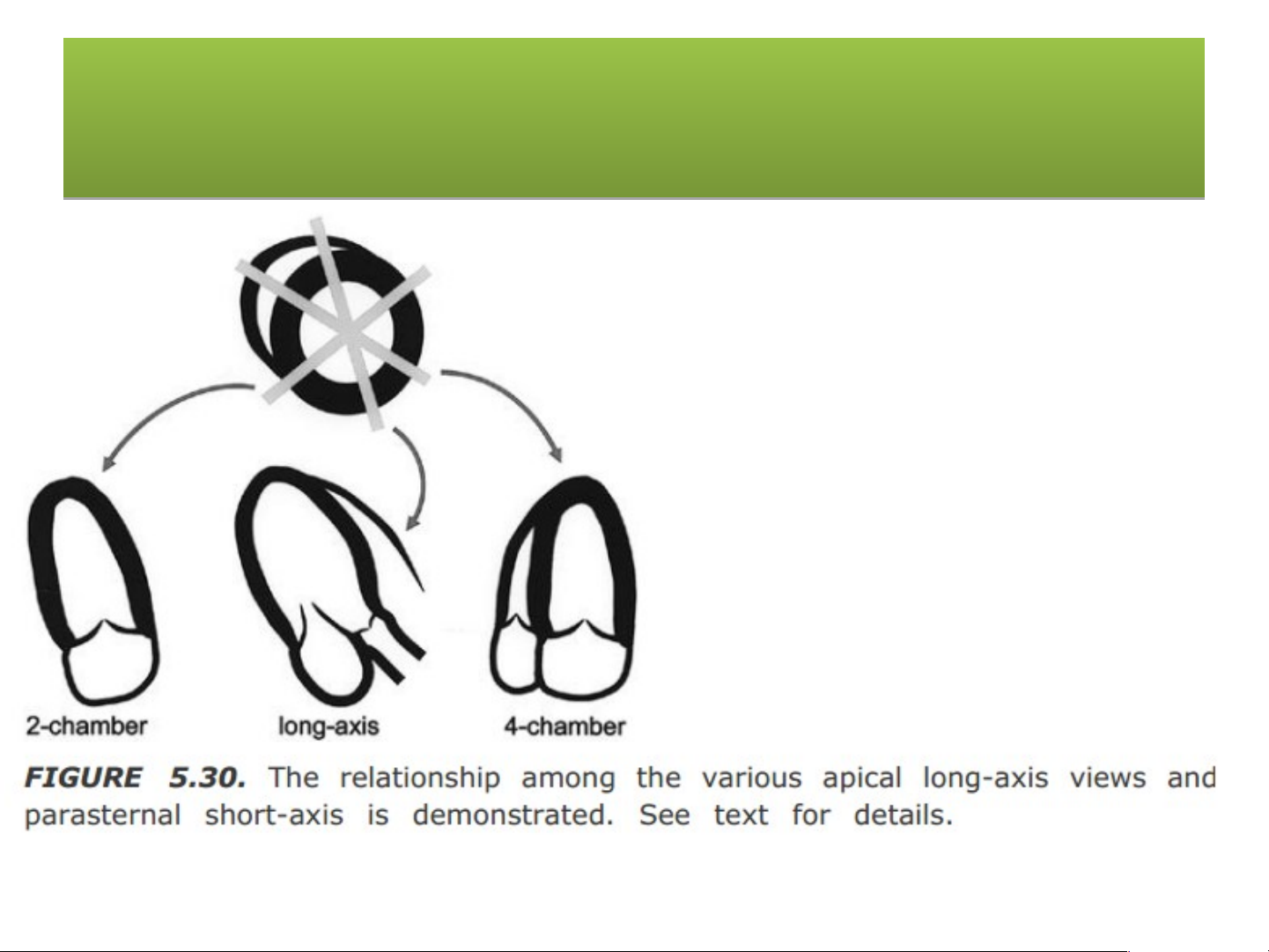
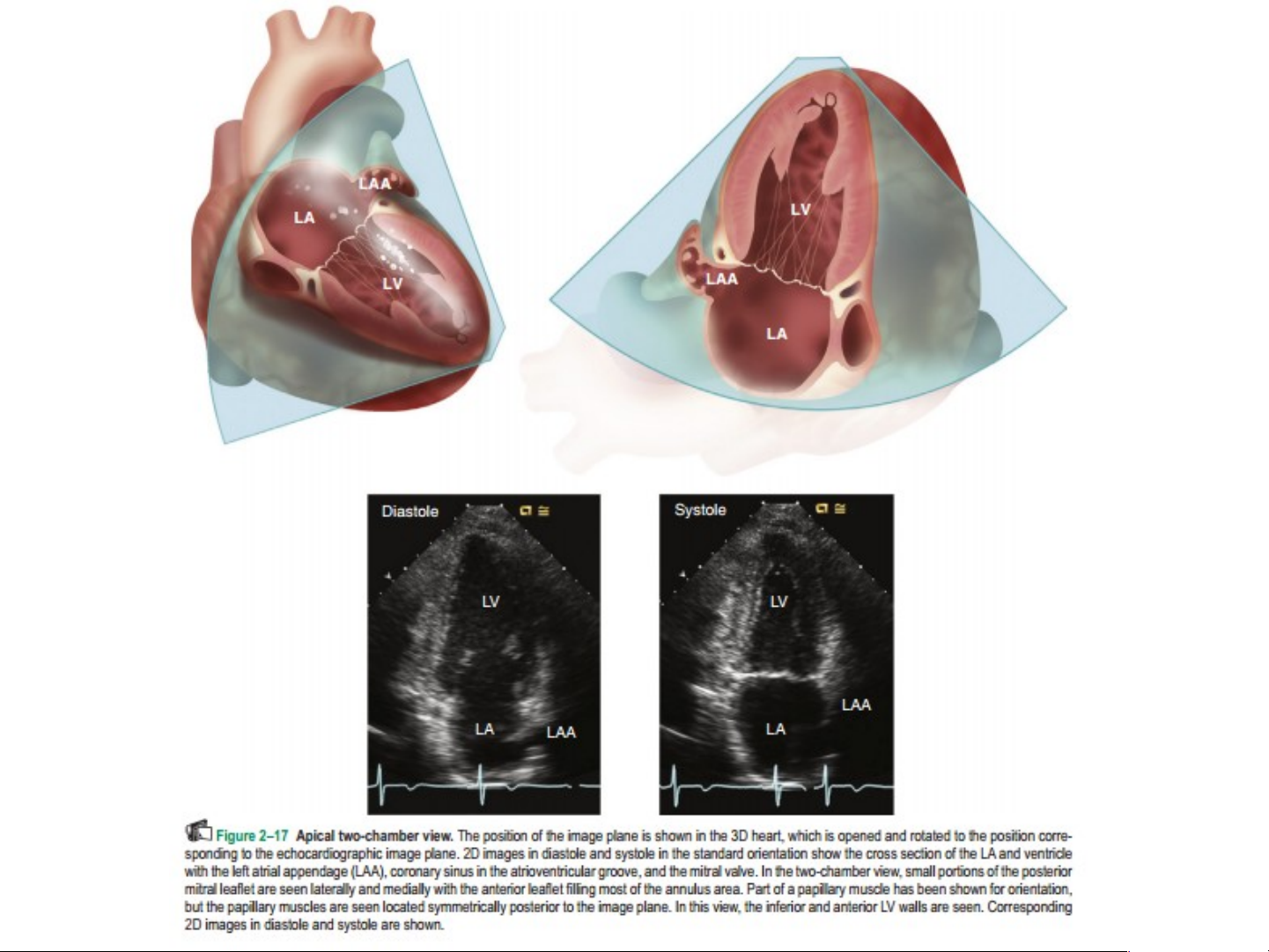
- 5. Two & Three Chamber View
- Slide 52
- Slide 53
- 6. Subcostal View
- Slide 55
- Slide 56
- Slide 57
- Slide 58
- Slide 59
- Slide 60
- Slide 61
- Slide 62
- Maët caét 5 buoàng döôùi söôøn
- Slide 64
- Mặt cắt quét dưới mũi ức trục dài
- Mặt cắt quét dưới mũi ức trục ngắn
- 7. Suprasternal View
- Slide 68
- Slide 69
- Slide 70
- 8. Right Parasternal View
- Tài liệu tham khảo
- Slide 73