Preview text:
JOURAL OF MEDICAL RESEARCH
DEPRESSION, AXIETY AND ASSOCIATED FACTORS
AMONG YOUNG PEOPLE DURING THE SECOND WAVE OF COVID-19 IN VIETNAM
Pham Phuong Mai1,2,*, Tran Nhu Hai1, Trinh Dinh Minh Viet2, Hoang Thi Hai Van1,2
1School of Preventive Medicine and Public Health, Hanoi Medical University
2Center for Training and Research on Substance Abuse and HIV
This cross-sectional study was conducted nationwide with a sample size of 9.781 participants in order to
describe the prevalence of depression and anxiety among Vietnamese youth (15-24 years old) during a COVID-19
outbreak and associated factors. The 21-item Depression, Anxiety and Stress Scale was used in this study.
Results showed that 10% of the Vietnamese youth exhibited mild to extremely severe depression and 15.6%
reported mild to extremely severe anxiety. Particularly, 1% of participants reported having severe or extremely
severe symptoms of depression and 2.6% having severe or extremely severe symptoms of anxiety. Being
christian or of other marital status or living in urban areas or having near poor or poor household income were
all associated with increased depression among young people. Meanwhile, youth who were female, of ethnic
minorities, Buddhist, Christian, or single, lived in urban areas, had only an elementary education, or had near
low or low household income reported more anxiety symptoms. Findings from this study call for appropriate
interventions to improve the mental health of the young population, especially in the context of COVID-19 pandemic.
Keywords: Depression, Anxiety, Youth, COVID-19, Vietnam. I. INTRODUCTION
Mental health disorders are considered
The prevalence of mental health disorders
major global health problems, with more than
is increasing among youth - 1 in 10 people
54 million people experiencing a variety of
reported experiencing at least one mental health
mental disorder symptoms.1 Mental disorders
problem.6 Findings from the U.S. National Survey
were estimated to account for 32.4% of years
from 2009 to 2017 showed that the incidence of
lived with disability and 13% of disability-
depression increased by 52% in the 2005 - 2017
adjusted life years.2 As of 2017, among a
period among adolescents aged 12 - 17, and
wide range of mental health concerns, anxiety
63% in 2009 - 2017 among young adults aged
disorders were the most common forms of
18-25.7 Approximately, 20% of adolescents may
psychopathology and depression was one of
experienced a mental health disorder each year.8
the leading causes of disability with more than
and 50% and 75% experienced problems before
264 million people affected globally.3 Notably,
the age of 14 and by the age of 24, respectively.9
these mental concerns are among the most
There exists little research on the
prevalent psychological concerns for young
prevalence of depression and anxiety among
people4 and they often occur in comorbidity.5
young people in Vietnam in recent years
Corresponding author: Pham Phuong Mai
despite evidence of COVID-19 impacts on
Hanoi Medical University
mental health. According to a study by the
Email: phamphuongmai@hmu.edu.vn
U.S. CDC, during the outbreak of COVID-19 Received: 27/01/2022
from August 2020 to February 2021, the Accepted: 13/03/2022
incidence of depression or anxiety increased JMR 154 E10 (6) - 2022 121 JOURAL OF MEDICAL RESEARCH
from 36.4% to 41.5% in seven days, mainly
Therefore, N ≥ 9312. Convenient sampling
among 18 to 29 years old.10 In Vietnam, little
was utilized to recruit participants in 2 months
is known about the prevalence of these mental
(from June 2020 to August 2020). Hanoi
disorders among youth during the COVID-19
medical students were trained to recruit and
pandemic. Extant literature while scarce,
conduct face-to-face interview using structured
rather focuses on the general Vietnamese
questionnaires at participants’ households in 12
population with predominant recruitment of
different provinces in Vietnam.
adult participants.11, 12 As such, we could find 2. Measures
only one study which highlighted approximately - Sociodemographic variables: were
9% of depressive and anxiety symptoms
composed of age, sex, ethnicity, marital status,
among Vietnamese young adults from 18 to 26
living area, education level, and economic status.
years old13 Still, there is insufficient evidence
on how commonly Vietnamese youth, defined
- Variables of depression and anxiety:
Previous research validated the use of DASS-
as between 14 and 25 years old by the World
21-V for Vietnamese adolescents, showing
Health Organization,14 experienceddepression
the scale’s adequate internal consistency and
and anxiety in a pandemic-related context.
convergent validity.15 18 DASS-21 is a 4-point
Therefore, this study aimed to describe
Likert scale (0 = ‘Did not apply to me at all-
the prevalence of depression and anxiety
Never’, 1 = ‘Applied to me to some degree, or
and associated factors among Vietnamese
some of the time–Sometimes’, 2 = ‘Applied to
young people during the second wave of the
me to a considerable degree, or a good part of COVID-19 pandemic in 2020.
time - Often’, 3 = ‘Applied to me very much, or
II. SUBJECTS AND METHODS
most of the time - Almost always’), consisting of
21 items. Of which, items 3, 5, 10, 13, 16, 17,
1. Study participants and Procedures
and 21 are for depression and items 2, 4, 7, 9,
This was a cross-sectional study using
15, 19, and 20 are for anxiety. According to the
Depression, Anxiety and Stress Scale (DASS-
scale, the subscale scores were calculated for 21) to measure the outcome.15
participants’ depression and anxiety by doubling
Eligible participants were those who were
the total scores in each subscale. Subscale
between 15 and 24 years old and could give
scores should range from 0-42. Participants
consent to participate in the study. People who
were categorized into different levels of clinical
were cognitively unable to give consent or severity:
answer questions were excluded from the study.
(1) Normal (0-9 for depression, 0-7 for anxiety);
To estimate the sample size, we used the
(2) Mild (10-13 for depression, 8-9 for anxiety); following formula:16
(3) Moderate (14-20 for depression, 10-14 for !(#$!) anxiety); N=Z2(1-α/2) &!
(4) Severe (21-27 for depression, 15-19 for In which: anxiety);
α (2-side significant level) = 0.1
(5) Extremely severe (≥ 28 for depression,
p (Expected proportion in population) = 0.03217 ≥ 20 for anxiety). d (absolute precision) = 0.003 3. Statistical Analysis 122 JMR 154 E10 (6) - 2022 JOURAL OF MEDICAL RESEARCH
Data was entered and analyzed by STATA 4. Ethical issues
16 software. Findings that followed normal
This study was conducted with the approval
distribution were reported in percentage, means,
of the Institute for Preventive Medicine and
and standard deviation. Logistic regression
Public Health as the practicum module. We
was used to assess the relationship between
obtained full consent from participants before
sociodemographic variables and depression
data collection. All identifiable information was and anxiety prevalence.
recoded to ensure the confidentiality. III. RESULTS
1. Sociodemographic characteristics of participants
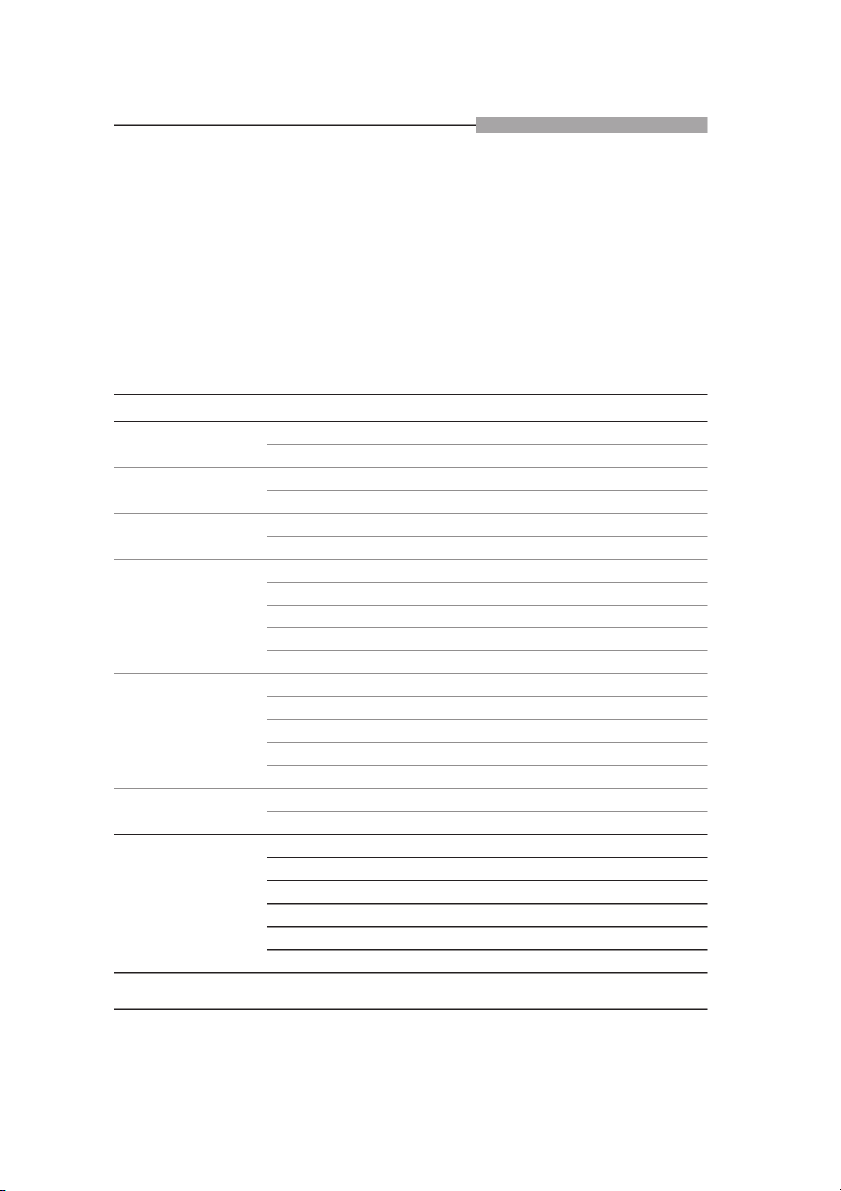
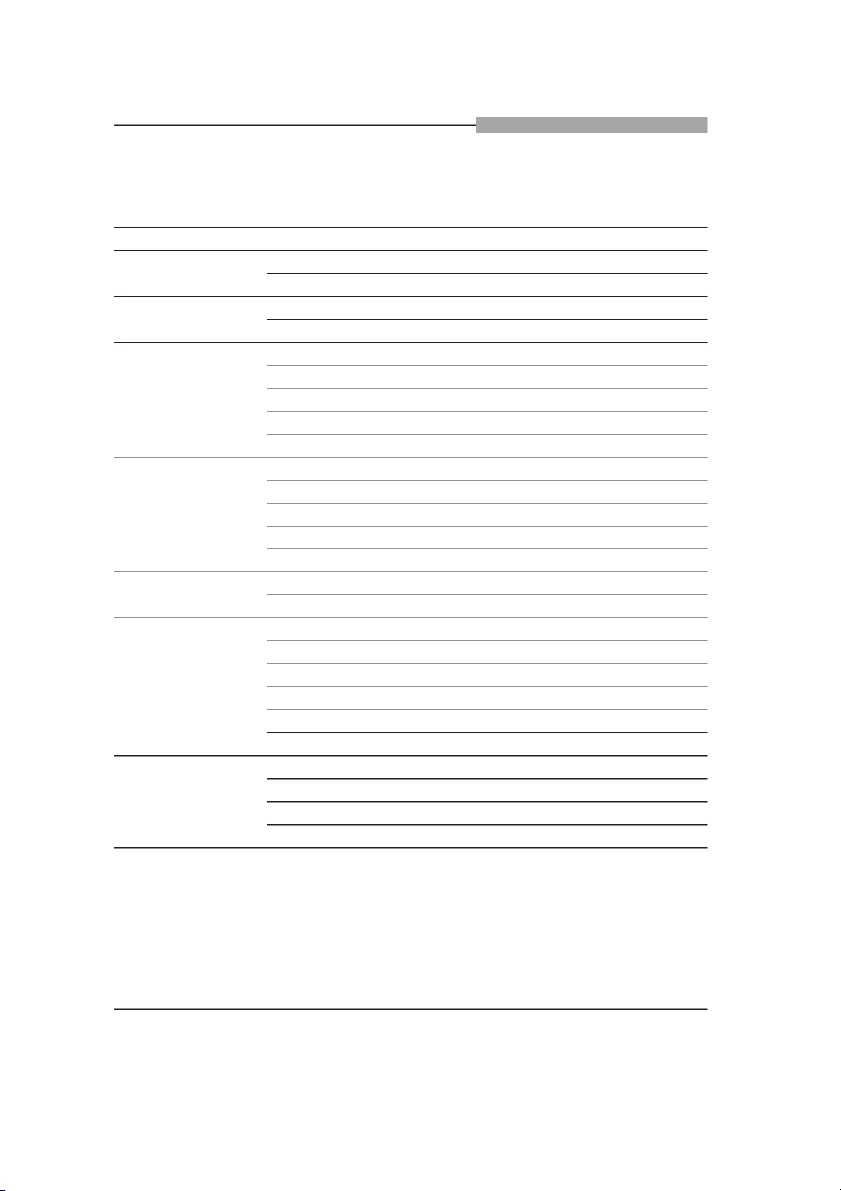
Table 1. Sociodemographic characteristics of participants (N = 9.781) n Percentage (%) 15 - 18 1.171 12.0 Age 19 - 24 8.610 88.0 Male 4.531 46.3 Sex Female 5.250 53.7 Kinh 9.309 95.2 Ethnicity Other 472 4.8 None 9.270 94.78 Buddhist 202 2.07 Religion Catholic 278 2.84 Christian 17 0.17 Other 14 0.14 Single 7.693 78.65 Married 2.006 20.51 Marital status Divorced/ Separated 36 0.37 Widowed 8 0.08 Other 38 0.39 Rural 4.866 49.75 Living area Urban 4.915 50.25 Elementary 21 0.21 Secondary 413 4.22 High school 2.436 24.91 Education Vocational 380 3.89 College/ University 6.429 65.73 Other 102 1.04 JMR 154 E10 (6) - 2022 123 JOURAL OF MEDICAL RESEARCH n Percentage (%) High 383 3.92 Middle 8.776 89.72 Household income Near poor 383 3.92 Poor 239 2.44
Table 1 described the sociodemographic
level while the smallest portion of the sample
characteristics of participants in our study
(2.44%) reported the in the low level.
(N=9.781). 88% were between 19 and 24
2. The prevalence of depression and anxiety
years old. The majority of participants were
among young people in Vietnam
female (53.7%). Most were Kinh, the most
2.1 Levels of depression and anxiety
common ethnicity in Vietnam (95.2%). 94.78%
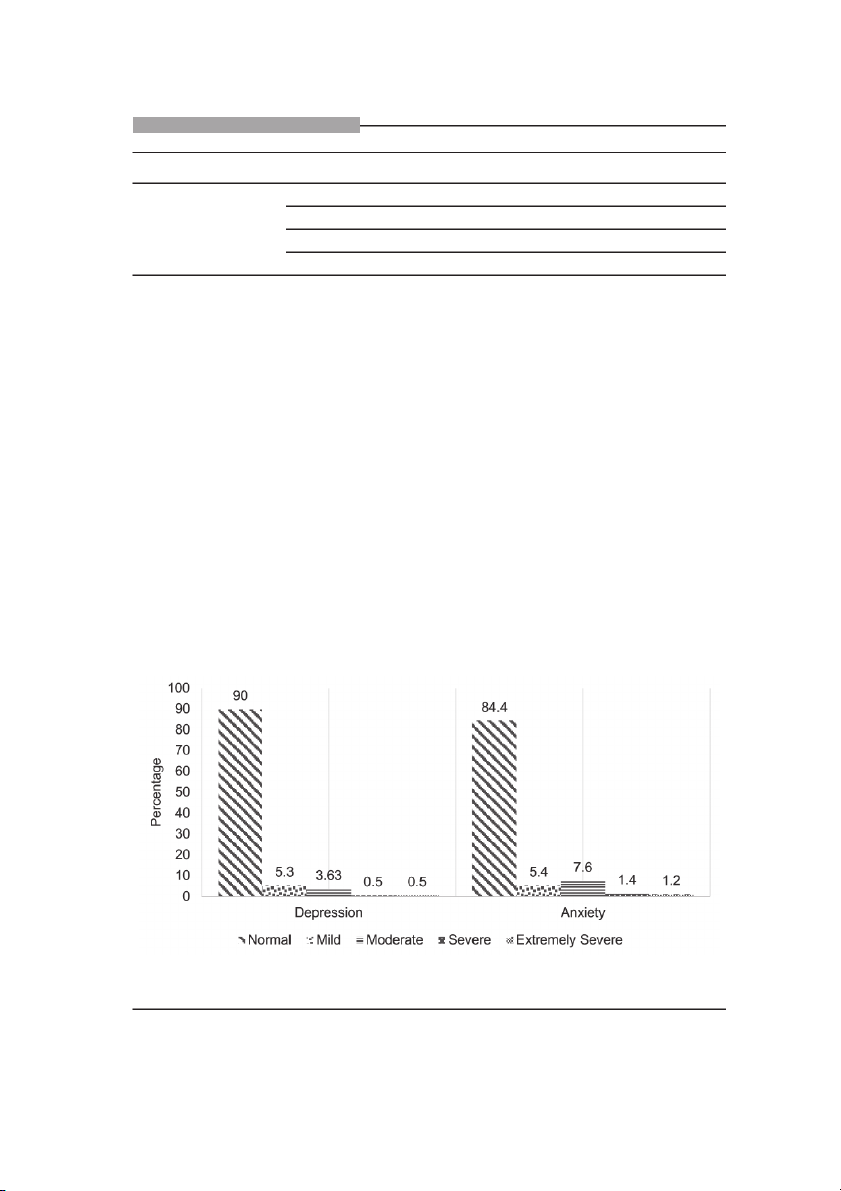
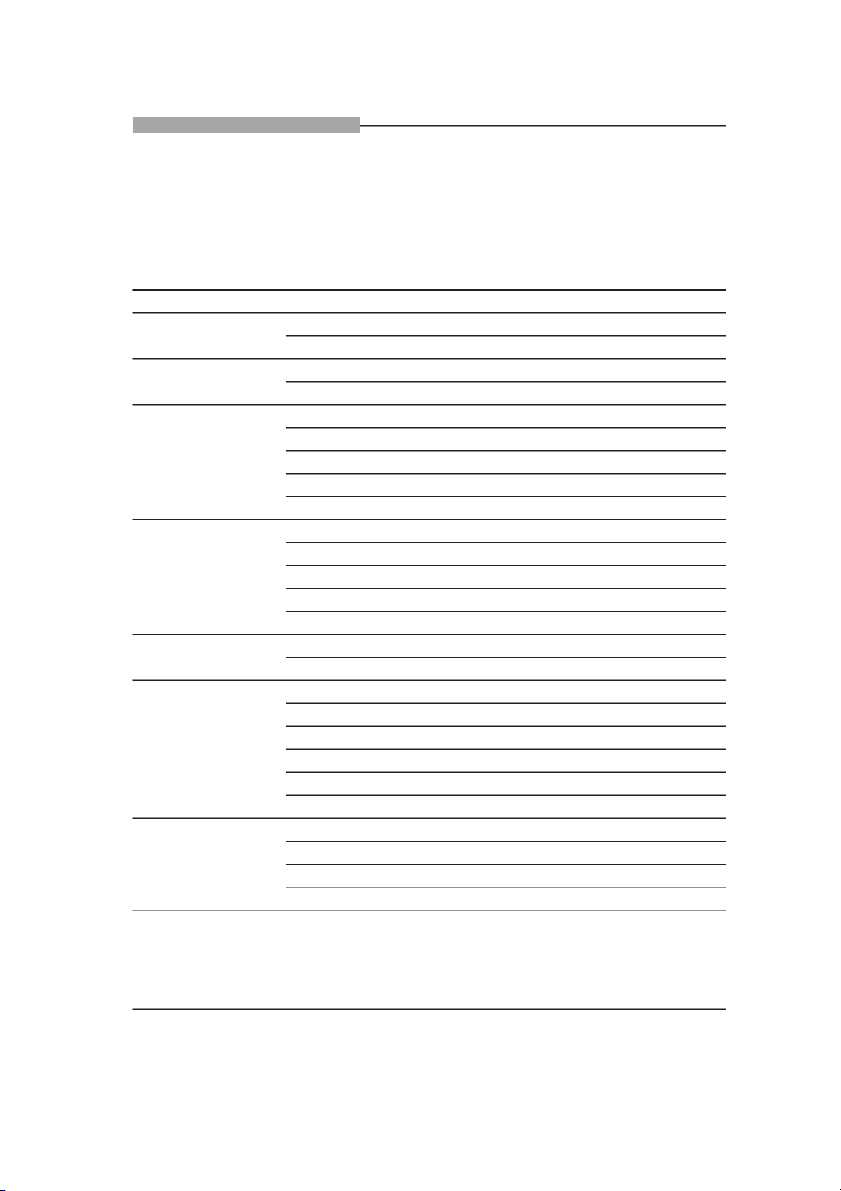
DASS-21 screening results showed that
of participants claimed no religion. Our sample
participants displayed relatively similar levels
included a relatively similar representation
of symptoms of depression (Mean=1.78) and
of Buddhists (2.07%) and Catholics (2.84%).
anxiety (Mean=1.77), suggesting moderate
Most participants reported to be single
severity of both disorders. Figure 1 illustrated
(78.65%). The distribution in terms of living
the prevalence of depression and anxiety
area was split with 49.75% living in rural areas
among young people in Vietnam. 15.6% and
and 50.25% in urban areas. A major portion
10% of participants reported mild to extremely
of our sample reported high education with
severe symptoms of anxiety and depression,
65.73% having graduated from a college or
respectively. Particularly, 1% showed severe
university and 24.91% having graduated from
to extremely severe depression while 2.6%
high school. In terms of household income,
reported severe to extremely severe anxiety.
89.72% of participants reportedin the middle
Figure 1. Levels of depression and anxiety among young people in Vietnam (N=9.781) 124 JMR 154 E10 (6) - 2022 JOURAL OF MEDICAL RESEARCH
2.2. Factors associated with symptoms of depression and anxiety among young people in Vietnam
Table 2. Factors associated with depressive symptoms (N = 9.781) n OR 95% CI Male 342 1 Sex Female 412 0.98 0.87 - 1.10 Kinh 707 1 Ethnicity Other 47 1.16 0.89 - 1.51 None 699 1 Buddhist 30 1.65 1.16 - 2.35 Religion Catholic 21 1.07 0.75 - 1.52 Christian 4 2.88 1.01 - 8.19 Other 0 1 - Single 645 1 Married 92 0.53 0.45 - 0.64 Marital status Divorced/Separated 5 1.49 0.65 - 3.41 Widowed 2 4.63 1.04 - 20.73 Other 10 2.51 1.24 - 5.09 Rural 337 1 Living area Urban 417 1.27 1.13 - 1.44 Elementary 2 1 Secondary 40 0.96 0.27 - 3.38 High school 191 0.85 0.25 - 2.90 Education Vocational 22 0.71 0.20 - 2.51 College/University 494 0.83 0.24 - 2.83 Other 5 0.57 0.14 - 2.33 High income 26 1 Middle income 611 1.11 0.79 - 1.55 Household income Near low 65 2.77 1.86 - 4.12 Low 52 3.64 2.38 - 5.58
Religion, marital status, living area, and
were 4.63 times more likely to have depression
household income were indicative of depressive
than single people. However, this finding was not
symptoms among young people. Logistic
significant because 95% CI was large, ranging
regression analysis results showed that
from 1.04 – 20.73 and the number of observations
Christians were 2.88 times more likely to have
for this category was small. On the other hand,
depressive symptoms than those with no religion
participants with other marital statuses (e.g., in a
(95% CI: 1.01 – 8.19). Those who are widowed
relationship) were 2.51 times more likely to report JMR 154 E10 (6) - 2022 125 JOURAL OF MEDICAL RESEARCH
depressive symptoms than single counterparts
having near low and low household income were
(95% CI: 1.24 - 5.09). Additionally, young people
3.64 and 2.77 times, respectively, more likely to
living in urban areas were 1.27 times more likely
report depressive symptoms than those having
to report depressive symptoms than those living
high household income (95% CI: 2.38 - 5.58,
in rural areas (95% CI: 1.13 - 1.44). Also, those 1.86 - 4.12).
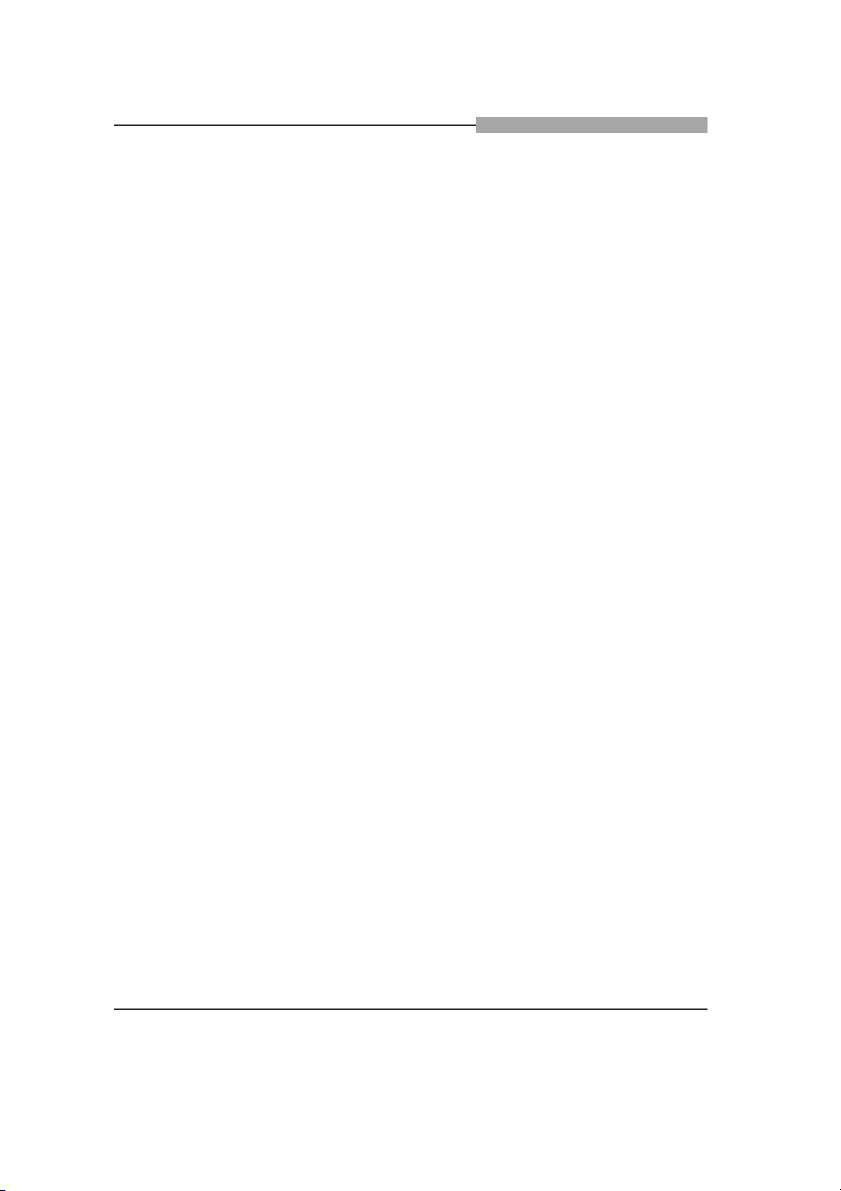
Table 3. Factors associated with the prevalence of anxiety (N=9.781) n OR 95% CI Male 733 1 Sex Female 994 1.21 1.08 – 1.34 Kinh 1.626 Ethnicity Other 101 1.29 1.02 – 1.61 None 1.607 1 Buddhist 61 2.06 1.52 – 2.79 Religion Catholic 50 1.04 0.77 – 1.43 Christian 8 4.23 1.63 – 11.0 Other 1 0.37 0.05 – 2.80 Single 1.471 1 Married 234 0.56 0.48 – 0.65 Marital status Divorced/Separated 7 1.02 0.48 – 0.65 Widowed 3 2.54 0.61 – 10.63 Other 12 1.95 0.98 – 3.87 Rural 768 1 Living area Urban 959 1.29 1.16 – 1.43 Elementary 6 1 Secondary 89 0.68 0.26 – 1.82 High school 446 0.56 0.22 – 1.45 Education Vocational 62 0.48 0.18 – 1.30 College/University 1.117 0.52 0.20 – 1.36 Other 7 0.18 0.05 – 0.62 High income 58 1 Middle income 1.490 0.14 0.86 – 1.52 Household income Near low 105 2.11 1.48 – 3.02 Low 74 2.51 1.70 – 3.71
Key indicators of anxiety symptoms among
participants were 1.21 times more likely to report
young people included sex, ethnicity, religion,
anxiety symptoms than male counterparts.
living area, education level, and household
Also, those of ethnic minorities were 1.29 more
income. Our findings suggested that female
likely to report anxiety symptoms than those of 126 JMR 154 E10 (6) - 2022 JOURAL OF MEDICAL RESEARCH
Kinh (95% CI: 1.24 - 5.09). In addition, religion
addition, sample size can also contribute to
was predictive of young people’s anxiety. In
the mentioned differences. Our large sample
fact, participants following Buddhism were
size (N = 9.781) was much larger than sample
2.06 more likely to report anxiety symptoms
sizes found in domestic and international
than those of no religion (95% CI: 1.24 – 5.09).
studies of the same topic. In addition, different
Participants who were Christian were 4.23 more
use of instrumentation can play a huge role in
likely to report anxiety symptoms than those of
incongruent prevalence rates. While the U.S.
no religion (95% CI: 1.63 -11.0). Those who
study measured the prevalence of depression
were married were twice less likely to report
and anxiety via DSM-IV criteria,19 we utilized
anxiety symptoms than those who were single
DASS-21 criteria instead. Yet, while our
(95% CI: 0.48 – 0.65). Participants residing in
findings did not replicate the prevalence
urban areas were 1.29 times more likely than
rates found in literature, they align with the
counterparts in rural areas (95% CI: 1.16 –
general consensus that the prevalence of
1.43). Additionally, those at higher education
anxiety symptoms is often higher than that of
levels (e.g., some high school, postgraduate) depressive symptoms.
were 0.82 times less likely to report anxiety
In our study, sex was a notable indicator of the
symptoms than those with elementary education
prevalence of anxiety symptoms among young
(95% CI: 1.16 – 1.43). Household income was
people in Vietnam during a COVID-19 outbreak.
also an important indicator of young people’s
In particular, though there was no sex difference
anxiety. Our results suggested that those with
in depression scores, female participants
low or near low household income were 2.11
were 1.21 times more likely to report greater
and 2.51 times, more likely than those with high
anxiety than male counterparts. In fact, the sex
income (95% CI: 1.48 – 3.02 and 1.70 – 3.71).
difference in anxiety symptoms in our study is IV. DISCUSSION
greater than that in a study in China of the same
To our knowledge, this was the first large-
year, which showed that female participants
who were between 12 and 18 years old were
scale study investigating the prevalence of
only 1.15 times more likely to report increased
depression and anxiety symptoms among
anxiety compared to male participants of the
young people in Vietnam, especially during a same age range.2 0 Age range may account for
COVID-19 outbreak. Our results showed that
this discrepancy. While the other study observed
the prevalence among this population was a more restricted age range,2 0 ours included a
15.6% for anxiety and 10% for depression.
broader measure of age (15-24).
Compared to young people in the United
States (14.3% for depression and 31.9%
Religion was also related to anxiety
for anxiety),19 though the prevalence rate
symptoms among young people in Vietnam.
of depressive symptoms in our study was
Our results indicated that, compared to those
relatively similar, anxiety symptoms was
with no religious affiliation, those who were
lower. This discrepancy can be explained by
Buddhist and Christian were at 2.06 times
the differences across samples. While the
and 4.23 times, respectively, greater odds of
U.S. study focused only adolescents aged
displaying anxiety symptoms. A different study
13 to 18,19 our study recruited participants
emphasized the relationship between increased
who were between 15 and 24 years old. In
religious behaviors and reduced depressive JMR 154 E10 (6) - 2022 127 JOURAL OF MEDICAL RESEARCH
and anxiety symptoms.21 Perhaps, our study
in China found that adolescents living in cities
did not replicate the mental health benefits of
had lower likelihood of reporting increased
religion due to the religious representation in
depressive and anxiety symptoms compared
our sample. While our sample was comprised of
to those living in rural areas (37.7% vs. 47.5%
mostly atheists (94.87%) and some Christians
and 32.5% vs. 40.4%).20 This discrepancy
(0.17%), other study recruited a major portion of
in findings may suggest that the role of living
Christians (73%) and a small portion of atheists
area may vary in prediction of the prevalence of
(11.5%) for their study sample.21
depression and anxiety among young people in
In addition, our study underscored the
Asia during the COVID-19 pandemic.
association between lower household income V. CONCLUSION
and increased depressive and anxiety
symptoms. Compared to those with high
Our study described the prevalence of
household income, young people with low
depressive and anxiety symptoms among
or near low household income were at 3.64
young people aged 15 to 24 in Vietnam during
times and 2.77 times, respectively, of reporting
the COVID-19 pandemic. We highlighted
depressive symptoms. For anxiety symptoms,
the correlation between sociodemographic
those with near p low and near low household variables and depressive and anxiety
income were 2.51 times and 2.11 times,
symptoms. Religion, other marital status,
respectively, more likely to report higher scores
metropolitan living, and near low or low
than those with high-tier household income.
household income were all related to young
According to a large study in Germany of 1586
people’s elevated depression. Also, we found
young people aged 7 to 18, low household
a positive relationship between female sex,
income was linked to migration background,
minority ethnicity, Buddhism, Christianity,
limited living space, and increased mental
single status, metropolitan living, elementary
health problems.22 Evidence in a different study
education level, near p low or low household
on young people’s mental problems during the
income and greater anxiety symptoms.
Such findings emphasize the needs for
COVID-19 pandemic suggests similar trends.23
As our findings support current literature, we implementing effective mental health
speculate that the relationship between family
interventions for Vietnamese young people
income and the prevalence of depressive and
enduring many COVID-19-related impacts.
Specifically, we recommended to develop
anxiety symptoms among young people during
the COVID-19 pandemic can be universal.
early intervention programs which target
young people who exhibit mild to extremely
Lastly, living area was also associated with
severe depression and anxiety with eclectic
how common depressive and anxiety symptoms
outlets for mental health care. Additionally,
were among the young population in Vietnam. further research, particular longitudinal
Our results indicated those who lived in cities
research should be conducted to investigate
were at 1.27 greater odds for reporting more
other social determinants of the prevalence
depression symptoms than those who lived in
of depression and anxiety, as well as stress,
rural areas. Similarly, compared to those in rural
and to examine the trends of depression and
areas, city dwellers were 1.29 times more likely
anxiety prevalence among young people over
to score higher in anxiety symptoms. A study
various COVID-19 waves in Vietnam. 128 JMR 154 E10 (6) - 2022 JOURAL OF MEDICAL RESEARCH REFERENCE
1. World Health Organization (WHO). Ngày
8. World Health Organization (WHO).
sức khoẻ tâm thần thế giới - một căn bệnh tiềm
Caring for children and adolescents with mental
ẩn. World Health Organization. https://www.who.
disorders: setting WHO directions. World Health
int/vietnam/vi/news/detail/09-10-2008-world-
Organization; 2003. https://apps.who.int/iris/
mental-health-day-a-hidden-illness. Published
handle/10665/42679. Accessed March 4, 2022.
October 9, 2008. Accessed March 6, 2022.
9. Kessler RC, Berglund P, Demler O,
2. Vigo D, Thornicroft G, Atun R. Estimating
et al. Lifetime prevalence and age-of-onset
the true global burden of mental illness. Lancet
distributions of DSM-IV disorders in the National
Psychiatry. 2016; 3(2): 171-178. doi:10.1016/
Comorbidity Survey Replication. Arch Gen S2215-0366(15)00505-2.
Psychiatry. 2005; 62(6): 593-602. doi:10.1001/
3. James SL, Abate D, Abate KH, et al. archpsyc.62.6.593.
Global, regional, and national incidence,
10. Vahratian A, Blumberg SJ, Terlizzi
prevalence, and years lived with disability for
EP, et al. Symptoms of anxiety or depressive
354 diseases and injuries for 195 countries and
disorder and use of mental health care among
territories, 1990–2017: a systematic analysis
adults during the COVID-19 pandemic - United
for the Global Burden of Disease Study 2017.
States, August 2020-February 2021. MMWR
The Lancet. 2018; 392(10159): 1789-1858.
Morb Mortal Wkly Rep. 2021; 70(13): 490-494.
doi:10.1016/S0140-6736(18)32279-7. doi:10.15585/mmwr.mm7013e2.
4. Bitsko RH, Claussen AH, Lichstein J, et
11. Le HT, Lai AJX, Sun J, et al. Anxiety and
al. Mental Health Surveillance Among Children
depression among people under the Nationwide
- United States, 2013-2019. MMWR Suppl.
Partial Lockdown in Vietnam [published
2022; 71(2): 1-42. Published 2022 Feb 25.
correction appears in Front Public Health. 2021 doi:10.15585/mmwr.su7102a1.
May 24;9:692085]. Front Public Health. 2020;
5. Ghandour RM, Sherman LJ, Vladutiu CJ,
8: 589359. doi: 10.3389/fpubh.2020.589359.
et al. Prevalence and Treatment of Depression,
12. Ngoc Cong Duong K, Nguyen Le Bao
Anxiety, and Conduct Problems in US Children.
T, Thi Lan Nguyen P, et al. Psychological
J Pediatr. 2019; 206: 256-267.e3. doi:10.1016/j.
impacts of COVID-19 during the first nationwide jpeds.2018.09.021.
lockdown in Vietnam: web-based, cross-
6.Mental Health Foundation. Children and
sectional survey study [published correction
young people. Mental Health Foundation.
appears in JMIR Form Res. 2021 Mar 5; 5(3):
https://www.mentalhealth.org.uk/a-to-z/c/
e28357]. JMIR Form Res. 2020; 4(12): e24776.
children-and-young-people. Published August doi:10.2196/24776.
7, 2015. Accessed March 4, 2022.
13. Porter C, Favara M, Hittmeyer A, et al.
7. Twenge JM, Cooper AB, Joiner TE, et al.
Impact of the COVID-19 pandemic on anxiety
Age, period, and cohort trends in mood disorder
and depression symptoms of young people in
indicators and suicide-related outcomes in a
the global south: evidence from a four-country
nationally representative dataset, 2005-2017.
cohort study. BMJ Open. 2021; 11(4): e049653.
J Abnorm Psychol. 2019; 128(3): 185-199.
doi:10.1136/bmjopen-2021-049653. doi:10.1037/abn0000410.
14. World Health Organization (WHO). JMR 154 E10 (6) - 2022 129 JOURAL OF MEDICAL RESEARCH
Adolescent mental health. World Health
e0180557. doi:10.1371/journal.pone.0180557.
Organization. https://www.who.int/news-room/
19. Merikangas KR, He JP, Burstein M, et
fact-sheets/detail/adolescent-mental-health.
al. Lifetime prevalence of mental disorders in
Published November 17, 2021. Accessed
U.S. adolescents: results from the National March 6, 2022. Comorbidity Survey Replication-Adolescent
15. Tran TD, Tran T, Fisher J. Validation of
Supplement (NCS-A). J Am Acad Child Adolesc
the depression anxiety stress scales (DASS) 21
Psychiatry. 2010; 49(10): 980-989. doi:10.1016/j.
as a screening instrument for depression and jaac.2010.05.017.
anxiety in a rural community-based cohort of
20. Zhou SJ, Zhang LG, Wang LL, et al.
northern Vietnamese women. BMC Psychiatry.
Prevalence and socio-demographic correlates
2013; 13(1): 24. doi:10.1186/1471-244X-13-24.
of psychological health problems in Chinese
16. Bartlett EJ, Kotrlik WJ, Higgins CC.
adolescents during the outbreak of COVID-19. Organizational Research: determining
Eur Child Adolesc Psychiatry. 2020; 29(6): 749-
appropriate sample size in survey research. Inf
758. doi:10.1007/s00787-020-01541-4.
Technol Learn Perform J. 2001;19:1. https://
21. Schapman AM, Inderbitzen-Nolan HM.
www.opalco.com/wp-content/uploads/2014/10/
The role of religious behaviour in adolescent
Reading-Sample-Size1.pdf. Accessed March
depressive and anxious symptomatology. J 4, 2022.
Adolesc. 2002; 25(6): 631-643. doi:10.1006/ 17. COVID-19 Mental Disorders jado.2002.0510. Collaborators. Global prevalence and
22. Ravens-Sieberer U, Kaman A, Erhart
burden of depressive and anxiety disorders
M, et al. Impact of the COVID-19 pandemic on
in 204 countries and territories in 2020 due
quality of life and mental health in children and
to the COVID-19 pandemic. Lancet. 2021;
adolescents in Germany. Eur Child Adolesc
398(10312): 1700-1712. doi:10.1016/S0140-
Psychiatry. doi:10.1007/s00787-021-01726-5. 6736(21)02143-7.
23. Guessoum SB, Lachal J, Radjack R, et
18. Le MTH, Tran TD, Holton S, et al.
al. Adolescent psychiatric disorders during the
Reliability, convergent validity and factor structure
COVID-19 pandemic and lockdown. Psychiatry
of the DASS-21 in a sample of Vietnamese
Res. 2020; 291: 113264. doi:10.1016/j. adolescents. PLOS ONE. 2017; 12(7): psychres.2020.113264. 130 JMR 154 E10 (6) - 2022




